What is Trench Mouth
Page Contents
Trench mouth is a rare bacterial infection characterized by ulcers, swelling, and inflammation of the gums. The condition got its name when soldiers in World War 1 were affected by severe gum problems as they were deprived of proper oral hygiene in the trenches.
The medical terms of this rapidly growing type of gingivitis are Vincent’s stomatitis, acute necrotizing ulcerative gingivitis (ANUG) and necrotizing ulcerative gingivitis. It is sometimes mistaken for a thrush or oral yeast infection.
Signs and Symptoms
Symptoms begin abruptly, with the earliest ones being:
- Bad breath
- Metal taste in the mouth
Other symptoms include:
Related to the Gums
- Excessive bleeding even with slight external pressure
- Gnawing pain
- Swelling
- Redness
- Development of crater-like sores between the teeth
- A covering of a grayish layer of dead tissues
Related to the Mouth
- Excess saliva production
- Pain while eating, talking or swallowing
Other Symptoms
- Uneasy feeling
- Sore throat
- Fatigue
- Mild fever
- Loss of appetite
- Lymph node swelling around neck, head and under jaw
What Causes Trench Mouth
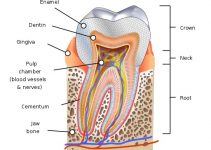
The mouth generally contains a balance of harmless bacteria, fungi and viruses. Trench mouth occurs when bacteria grows abnormally and damages the gum tissues (gingiva).
The exact mechanism of bacterial infection is not known, but it’s assumed that certain enzymes, as well as toxins produced by the bacteria may be responsible.
Is Trench Mouth Contagious
Trench mouth is not contagious but it is a serious condition that needs immediate attention.
Risk Factors
It can occur in both adults and children, but is more likely to affect people between 15‑ 35. Developing countries with malnourishment and poor oral hygiene are also at risk. The other factors include:
- Recurring infection of tooth, mouth or throat
- Vitamin deficiencies (especially vitamins B and C)
- Emotional stress
- Smoking
- Diabetes
- Weak immune system
- HIV/AIDS
Complications
- Mouth ulcers
- Tooth loss
- Dehydration
- Gangrenous stomatitis
- Peritonitis
- Toxemia
- Vincent’s angina
How to Prevent Trench Mouth
Trench mouth is a rare ailment and can be prevented by avoiding the risk factors. Practicing some good habits like the following can help reduce the chances of developing the infection:
- Abstaining from smoking or chewing tobacco
- Practicing some stress relief techniques like yoga and exercise for minimizing stress
- Going to the dentist for a professional oral cleaning once every six months
Tests and Diagnosis
The doctor may order the following tests if trench mouth is suspected:
- A detailed clinical examination of teeth and gums
- Dental X-ray to determine the severity of the infection and to see how much tissue has been damaged
- Blood tests to find out the type of bacteria causing the damage
- Throat swab culture test for further confirmation of the condition
Differential Diagnosis
- Adrenal insufficiency and adrenal crisis
- Allergic reaction
- Fungal infection
- Blood dyscrasias
- Chronic debilitating disease
- Gingivitis diabetes mellitus
- Gingivitis, desquamative
- Gingivitis pregnancy
- Gingivitis, phenytoin
- Glossitis
- HIV/AIDS-related periodontitis
- Inadequate plaque removal
- Noma (cancrum oris)
- Pericoronitis
- Periodontitis
- Yeast
Trench Mouth Treatment
The treatment, directed at curing the infection and relieving the symptoms, is carried out on the basis of which stage the infection has reached and whether severe symptoms and complications like fever or enlargement of lymph nodes have developed.
Home Remedies to Get Rid of Trench Mouth
In the early stages of the infection, rinsing with salt water, chlorhexidine or a hydrogen peroxide solution can help in softening sore gums and in removing dead tissues. Baking soda may also be used for rinsing since it may prevent the infection from spreading.
Medication to Prevent the Infection from Spreading
In more serious cases, Antibiotics such as such as amoxicillin, erythromycin, and tetracycline can prevent the infection from spreading further, especially where a professional cleaning is not done immediately.
Professional Cleaning
For relatively mild infections with little or no complications, a thorough cleaning of the gums is achieved after three successive sittings. In the first, superficial deposits of plaque are removed by using ultrasonic scalers. In the second and third, root planning and scaling are done.
In case there are complications present, the primary cleaning procedure may also involve removal of a gray substance covering the affected gums, using a cotton dipped in hydrogen peroxide.
Medicines such as penicillin or metronidazole may also be prescribed following the cleaning, along with instructions to rinse the mouth with a 3% diluted hydrogen peroxide once every 2 hours during the healing period. If the condition of the gums gradually recovers, ultrasonic scalers are used to remove superficial deposits in later visits, while over-the-counter pain relievers like lidocaine are recommended to minimize pain.
Surgery for Severe Infection
If a pocket or abscess develops deep in a tissue, reconstructive and corrective surgeries may be necessary to open up the area and remove the dead, infected tissues.
Follow-up Measures
Once the treatment is complete, the patient needs to maintain proper oral hygiene to avoid any recurrence. Here are a few things that are commonly recommended in the follow-up treatment:
- Daily brushing
- Flossing
- Using a proper antibacterial mouthwash regularly
- Drinking lots of water
- Avoiding food irritants like hot and spicy food
- Proper nutrition with sufficient vitamin B- and C-rich foods
- Exercise and yoga to avoid stress
Prognosis
The condition can be cured with proper treatment and oral measures, but if left untreated, it may spread to tongue, cheeks, lips, and even the jaw bone, requiring major surgeries. Such severe cases may also interfere with the normal lifestyle of the affected person on a long run.
How Long Does Trench Mouth last
In most cases, the recovery time necessary is no more than a few weeks, but it is rather painful till treated.
Trench Mouth ICD-9-CM Codes and ICD-10-CM Codes
The ICD-9-CM code of Trench Mouth is 101, and ICD-10-CM code is A69.1.