Retinopathy of prematurity (ROP) is a proliferative disorder of the eye and is one of the few causes of visual impairment during childhood. Read and know all about the symptoms, causes, diagnosis, treatment and more about this visual disability.
Retinopathy of prematurity Definition
Page Contents
- 1 Retinopathy of prematurity Definition
- 2 Retinopathy of prematurity Classification
- 3 Retinopathy of prematurity Symptoms
- 4 Retinopathy of prematurity Causes
- 5 Retinopathy of prematurity Diagnosis
- 6 Retinopathy of prematurity Guidelines
- 7 Retinopathy of prematurity Differential Diagnosis
- 8 Retinopathy of prematurity Treatment
- 9 Retinopathy of prematurity Risk factors
- 10 Retinopathy of prematurity History
- 11 Famous people with Retinopathy of prematurity
It is a congenital condition characterized by an abnormal development of blood vessels in the retina and vitreous of the eye. Normal growth of the retinal blood vessels may begin 3 months after conception. In normal individuals, development is complete at the time of birth. In this condition, however, the development is entirely disrupted in infants who are born before 31 weeks of gestation. Areas of fibrous tissue, known as scars, develop on the retina and frequently give rise to bleeding. ROP is generally manifested by mild symptoms. However, it may result in complete vision loss in serious conditions.
Retinopathy of prematurity Classification
The International Classification of Retinopathy of Prematurity (ICROP), which was published in 1984, used certain criterions to describe the condition. Physicians normally refer to ICROP for the purpose of screening. Some of the essential parameters defined are:
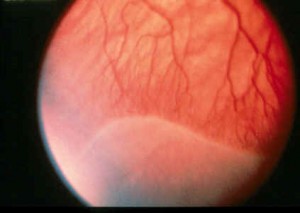
Picture 1 – Retinopathy of prematurity
Zones
There are 3 concentric zones on the retina where each one of them is centrally located on the optic disc or optic nerve head. Normal development of the retinal vessel usually begins from the center of the optic disc and proceeds towards the extreme periphery of the retina.
Zone 1
It is the posterior region of the retina that appears as a circle. Its radius extends twice the distance from the optic nerve to the macula – an oval-shaped yellow spot near the center of the retina. ROP is found to be extremely critical in this region.
Zone 2
It is in the form of a ring where the inner border is represented as Zone 1. On the other hand, the outer border has a radius equivalent to the distance between the optic nerve and nasal ora serrata. ROP in this zone is moderate, but may quickly progress to the primary zone within 1-2 weeks.
Zone 3
It forms the temporal crescent of retina anterior to Zone 2. The condition is in the dormant state and is marked by absence of any symptoms.
Circumferential extent
The parameter represents the degree of spread of ROP. In this case, the eye is presumed to be divided into twelve sections identical to a clock. It generally ranges from 1 to 12 hours. The extent of the disorder is defined by how many clock hours of the circumference of the eye are affected. This is, however, not a very important method for detection.
Stages
There are five stages of ROP that range from mild to severe.
Stage 1
In this phase, the blood vessels have a growth that is abnormal yet subtle. The disorder does not undergo any further progression and gets resolved on its own. Affected patients do not require any treatment and can regain normal vision.
Stage 2
The anomalous growth of retinal vessels occurs at a very moderate rate. It is quite similar to stage 1 where sufferers can revive normal vision.
Stage 3
It is characterized by severe abnormal blood vessel growth towards the center of the eye. It is also manifested by an extraretinal fibrovascular tissue. Infants who develop Plus Disease (a condition marked by enlargement and twisting of the retinal blood vessels, indicating a worsening of the disorder) at this stage should be considered for early treatment. Plus Disease can be detrimental to the eye. Treatment at this stage can prevent retinal detachment.
Stage 4
There is a partial detachment of retina. Severely developed abnormal blood vessels pull the retina away from the posterior wall of the eyeball. The tearing of the scar tissues on the retina can also cause retinal detachment along with profuse bleeding.
Stage 5
This is the final and the most serious stage of ROP that could lead to complete retinal detachment. If treatment is not sought at this level a total loss of vision may occur.
Retinopathy of prematurity Symptoms
As already said, this condition is generally asymptomatic. However, it may exhibit some symptoms under critical conditions like:
- Crossed eyes
- Extreme nearsightedness
- Involuntary eye movements
- White pupils
Retinopathy of prematurity Causes
Medical experts are not completely aware of the exact cause of ROP. The circumstances that lead to disorganized growth of blood vessels at a nascent stage of development are normally not found to have any genetic link.
Premature birth can prevent complete growth of the retinal blood vessels and become a possible cause of ROP. Due to this reason, the blood vessels are unable to reach the periphery of the retina and result in poor supply of oxygen and nutrients. Undernourishment of the peripheral retina could give rise to abnormal blood vessel growth while trying to reach other sources for nutrients.
Retinopathy of prematurity Diagnosis
The condition demands a thorough physical examination of the eye of an affected infant. It basically involves a proper assessment of the extent of growth of abnormal retinal blood vessels. Further evaluation is not mandatory if ROP is located at Zone 3.
Indirect ophthalmoscopy of the retina is performed to produce an inverted image of high magnification. Scleral depression is mandatory to view the peripheral regions of the retina.
Retinopathy of prematurity Guidelines
The Canadian Ophthalmological Society, the Canadian Association of Pediatric Ophthalmologists and the Canadian Pediatric Society have recommended the following guidelines that must be adhered to while screening a patient:
Risk group
- Infants should be of 3-4 weeks after birth or 31 weeks of gestation
- Infants should have a birth weight 1500 grams or less
Examiner
An experienced ophthalmologist should be consulted for appropriate diagnosis of ROP.
Schedule of assessments
- The frequency of examination generally depends on the severity of the disorder
- Weekly examination is necessary for patients who suffer from Plus Disease or have ROP in Zone 1 or Stage 3
- Examinations should be done on a continuous basis until the retina is sufficiently vascularized in Zone 3 or has completely resolved
- The exact state of an infant’s eye should be well-documented in accordance with the terms of the ICROP during each test
- Recommendation should also be given in order to know when the next examination should be performed
- The concerned physician must forward this information to the other person who will be conducting the next test
Responsibility
- The exact state of an infant’s eye should be well-documented in accordance with the terms of the ICROP during each test
- Recommendation should also be given in order to know when the next examination should be performed
- The concerned physician must forward this information to the other person who will be conducting the next test
Follow-up
Regular follow-up should be done 2 weeks after every examination to detect any further progression of the disorder.
Retinopathy of prematurity Differential Diagnosis
ROP should be distinguished from other conditions that produce similar symptoms. Some of them include:
- Familial exudative vitreoretinopathy
- Persistent Fetal Vascular Syndrome
Retinopathy of prematurity Treatment
Physicians usually begin the treatment within 72 hours of the eye exam. Some of the major therapeutic options include:
Laser photocoagulation surgery
The avascular retina (retina without blood vessels) can be easily destroyed through cauterization, using a laser. In this technique, the abnormal ocular blood vessels are burnt to prevent severe blood loss and growth.
Cryotherapy
Retinal destruction is carried out using an instrument to freeze the peripheral regions of the retina. This particular method not only destroys the affected areas, but may also delay or reverse the abnormal growth of blood vessels.
Vitrectomy
The vitreous gel that fills the space between the lens and retina of the eyeball is often replaced with a saline solution. The scar tissues formed on the retina are peeled off or excised after the removal of vitreous gel. In this way, the retina is brought nearer to the eye wall. It is generally utilized at stage 5.
Scleral buckling
This is one of the most effective ophthalmologic procedures that can repair a retinal detachment. In this method, a thin silicone band is placed around the sclera – an opaque, fibrous, outer layer of the eye. This in turn causes the wall of the eye to come closer to the detached retina. The encircling silicone band also obstructs the vitreous gel from touching the scar tissues. It is usually performed at stage 4 or 5 of ROP.
Bevacizumab (Avastin)
This is a very common drug that is generally used to slow the growth of new vessels. It is administered to the affected individuals, intravitreally (via an eye) to prevent the abnormal growth in retina.
Retinopathy of prematurity Risk factors
Low birth weight is likely to increase the chances of ROP in premature infants. In addition to this, there are other determinants that could lead to retinal detachment such as:
- Infection
- High carbon dioxide content in the blood
- Cardiac disorders
- Low blood oxygen
- Acute respiratory distress
- Brief pauses in breathing
- Low blood pH
- Slow heart rate
- Blood transfusion
Retinopathy of prematurity History
A worldwide epidemic of ROP was seen during 1941-1953. In 1941, a premature infant in Boston was diagnosed with ROP on St. Valentine’s Day. Although many such cases were seen all over the world, the cause was unknown. Developed countries with good health care facilities were, in fact, the most affected. Some British scientists inferred that oxygen toxicity was the cause of this condition. A few American pediatricians conducted a study, involving two groups of babies. Some of them were administered with oxygen in their incubators. The remaining group was given low oxygen supply. The latter group was observed to have a lower incidence of the disorder. Pediatricians finally arrived at the conclusion that the epidemic could be prevented by lowering the oxygen levels in incubators.
Famous people with Retinopathy of prematurity
Some well-renowned personalities who are presently suffering from ROP include:
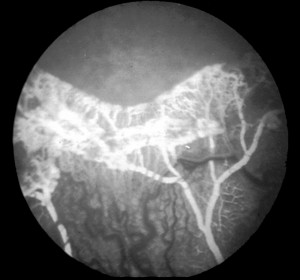
Picture 2 – Retinopathy of prematurity Image
- Stevie Wonder
- Tom Sullivan
- Diane Schuur
Retinopathy of prematurity is not a serious ophthalmologic disorder and is curable. It is very important for an ophthalmologist to determine the zone as well as the stage of the condition. In most cases, patients tend to recover without any form of treatment. However, if the ocular disorder has reached a vital state, immediate medical aid should be availed.
References:
http://en.wikipedia.org/wiki/Retinopathy_of_prematurity
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002585/
http://www.nei.nih.gov/health/rop/rop.asp#1
http://www.nlm.nih.gov/medlineplus/ency/article/001618.htm