Pleurisy is a highly painful lung condition that causes acute discomfort in sufferers, often limiting normal activities at times. Find out all about this disorder, including its causes, symptoms, treatment, prognosis and more.
What is Pleurisy?
Page Contents
- 1 What is Pleurisy?
- 2 Pleurisy ICD 9 Code
- 3 Pleurisy Symptoms
- 4 What Causes Pleurisy?
- 5 Pleurisy and Lupus
- 6 Pleurisy Diagnosis and Testing
- 7 Pleurisy Differential Diagnosis
- 8 Pleurisy Treatment
- 9 Pleurisy Home Remedies
- 10 Pleurisy Complications
- 11 Pleurisy Prognosis
- 12 Pleurisy Follow-Up and Monitoring
- 13 Prognosis Prevention
It refers to a swelling of the pleura or the lining of the chest and the lungs that usually gives rise to a piercing pain when sufferers cough or even breathe.
The condition is also known as “Pleuritis” or “Pleuritic chest pain.”
Pleurisy ICD 9 Code
The ICD 9 Code for this disorder is 511.
Pleurisy Symptoms
The condition mainly gives rise to painful sensations in the chest of patients. Sufferers usually experience aches while coughing or while taking a deep breath. Some patients experience painful symptoms in the shoulder. The aches may get worse with coughs, deeper breaths (due to exertion) and chest movement.
Picture 1 – Pleurisy
The disease may also lead to the accumulation of fluid inside the chest cavity. This can cause difficulties while breathing and may give rise to the following health issues:
- Coughing
- Cyanosis or bluish discoloration of skin
- Tachypnea or rapid breathing
- Chills, fever and loss of appetite (based on the cause)
- Respiratory shortness
In case of a fluid accumulation (referred to as Pleural effusion), the aches generally resolve as the fluid acts as a lubricant. However, accumulation of too much fluid can exert pressure over the lungs and compress it – thereby impairing its normal functioning. This leads to a shortness of breath. In case the fluid gets infected (Empyema or infected Pleural effusion), various discomforting symptoms such as chills, fever and dry cough may occur.
Certain sufferers experience relief from pain when they apply pressure over the aching region or hold their breath.
What Causes Pleurisy?
The pleura (a double layer of membranes) separate the lungs from the chest wall. One layer of this membrane lies over each lung while the other layer lines the inner wall of the chest. The layers appear as two smooth satin strips rubbing against each other, not causing any friction. This allows the lungs to expand and contract while breathing without any resistance from the chest wall.
When they suffer an inflammation, the two pleural membrane layers in the impacted side of the chest rub against one another like two strips of sandpaper. This can cause aches when a person breathes in and out.
This inflammation of the pleural membranes may occur due to a number of factors, such as:
- Infectious disorders, such as Tuberculosis
- Influenza and other severe viral infections
- A clot in a lung artery (Pulmonary embolism)
- Pneumonia, in cases where the infected lung region involves the pleural surface
Pleuritis may also result from:
- Cardiac surgery
- Chest trauma
- Lupus
- Rib fractures, such as those occurring due to severe cough
- Lung cancer (in rare cases)
- Rheumatoid arthritis
- Conditions related to Asbestos-exposure
Smoking has not been stated as a direct cause of the disorder. However, “smoker’s cough” has been found to worsen the painful sensations associated to the disorder. Some cases of Pleuritis are idiopathic, meaning their underlying causes are not known.
Pleurisy and Lupus
Systemic lupus erythematosus (SLE) is the name given to an autoimmune condition that attacks the immune system of the body and affects everything from the joints to the skin of patients. It can frequently trigger an inflammation in the pleura (lining around the lungs) and give rise to Pleurisy. Pleuritis is common in patients of Lupus. Around 30-60% of all Lupus sufferers are estimated to suffer from a pleural inflammation at some time in their lives.
Pleurisy Diagnosis and Testing
The pleura that line the lungs are normally smooth in appearance. In patients of Pleuritis, the surface of this lining becomes rough. The membranes rub together with each inhalation of the sufferer and mar produce a grating noise known as ‘friction rub.’ A doctor investigating Pleurisy places his stethoscope or his ear against the chest of his patient to listen to this sound. The presence of this sound confirms the condition. However, this ‘friction rub’ or ‘snow crunching’ sound is not always present. It is due to this reason that various diagnostic tests are recommended to patients of the condition. These include:
Thoracentesis
It involves injecting a local anesthetic into the area between the ribs where a fluid accumulation has occurred. A needle is then inserted into the region to extract some of the fluid and send it for laboratory analysis. In cases where only a small amount of fluid is present, the needle may be guided with ultrasound.
Pleural biopsy
This is usually recommended if a physician suspects lung cancer or tuberculosis to be the underlying cause. It includes removal of a sample of tissue with the aid of a hooked needle and using it for pathological analysis in a laboratory setting. Like in Thoracentesis, ultrasound may be used in this technique too for better diagnosis.
Thoracoscopy
It is carried out when patients are under the effects of a general anesthetic. The process involves observing the inner region of the chest and obtaining a sample of pleural tissue. A surgeon makes a single or multiple incisions between the ribs and inserts a tube fitted with a small video camera. The technique is sometimes referred to as Video-assisted Thoracoscopic Surgery (VATS).
CT scan of the chest
Computerized Tomography (CT) scan is usually the first imaging exam used by physicians for diagnosing this disorder. It helps doctors look for any abnormality in the thin chest sections. In this exam, a computer renders highly detailed images of the chest sections – thus helping doctors detect and analyze abnormalities more easily.
Chest X-ray
It helps reveal a swollen region of the lungs that suggests Pneumonia. In some cases, a special type of chest X-ray is used. Patients are made to lie on the side of the Pleurisy to check whether any fluid, that is not apparent on a standard chest X-ray, is present. This is known as “Decubitus chest x-ray.”
Chest ultrasound exam
In this imaging examination, high-frequency audio waves are used to render accurate images of internal structures. A physician may use this process to find out whether there is a pleural effusion.
CBC (Complete Blood Count)
A blood test helps doctors know whether a patient is suffering from an infection, and in case he is – what type of an infection it is. Blood exams may also reveal whether there is an underlying autoimmune condition, such as lupus or rheumatoid arthritis. Pleuritis is often an initial sign of such disorders.
The medical history of a patient is also taken into consideration. It is noteworthy that Pleuritis is often diagnosed only when a doctor has ruled out other causes of a more acute nature.
Pleurisy Differential Diagnosis
The differential diagnosis of Pleuritis involves ruling out other possible causes of chest pain, such as Angina. Such diagnoses are often deemed as necessary to confirm detection. This is because even with advanced x-ray exams, it is not always easy to visualize Pleurisy.
Pleurisy Treatment
It is necessary to seek treatment on an emergency basis in case of respiratory difficulties, acute pain or violent coughs. Some cases of chest pain are dangerous and even experienced physicians are sometimes unable to detect the exact cause for pain.
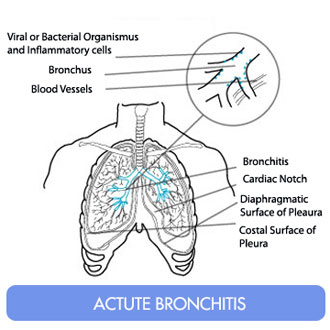
Picture 2 – Pleurisy Image
The treatment of this disease depends on its underlying cause. While antibiotics are used for treating bacterial infections, an operative technique may be needed to drain infected fluid from the affected lungs of a patient. Viral infections generally subside without the use of medicines. Anti-inflammatory drugs (like Ibuprofen) or Acetaminophen are often used by patients themselves to control the painful symptoms associated with this disorder. Prescription or over-the-counter NSAIDs (non-steroidal anti-inflammatory drugs) may provide relief from certain symptoms of the disease. Painful symptoms and coughs may be controlled with the aid of a prescription Codeine.
In case of accumulation of large amounts of fluid, patients may require a hospital stay. During this period, a tube is usually inserted into the chest to let the fluid drain away constantly. Hospitalization is often required to keep a close watch on the respiratory stability of sufferers.
Pleurisy Home Remedies
Unfortunately, the disorder cannot be cured with the aid of simple home remedies. However, adopting certain steps for lifestyle management can help sufferers get relief from the symptoms associated with the disease. These include:
- Using over-the-counter medicines, such as Motrin and Advil, to get relief from associated inflammation and pain
- Taking a lot of rest, even while feeling better. Proper rest and restricting activities can promote healing
- Lying on the painful side, which can actually reduce the aches
Pleurisy Complications
The disorder does not usually give rise to any severities other than acute pain, as reported by some patients. However, the pain can be quite severe and debilitating for patients. Such intense aches may limit activities and the ability to work. Patients may even find themselves unable to perform even simple jobs.
It is only in rare cases that complications are found to occur. The usual problems arising due to this syndrome involve those arising from the original cause as well as other associated problems like:
- Respiratory difficulties
- Lung collapse, as a result of Thoracentesis
Pleurisy Prognosis
The outcome of the condition and recovery from it actually depends on its underlying cause. Prognosis also depends on the severity of the disorder. Unfortunately, individuals affected by the condition take several months to recover. When viral infections are the cause, the disorder generally resolves after a week. However, the condition may continue for an indefinite period of time if it arises due to cancerous syndromes. Even with proper treatment, the disease may persist for a few months and become difficult to be treated successfully. It may cause much pain to affected individuals.
Pleurisy Follow-Up and Monitoring
The condition gives rise to acute discomfort. Unless the painful symptoms are properly managed, patients may develop Pneumonia. This is due to their inability to breathe and cough in a proper manner. If the painful sensations turn worse after a week, despite use of proper medications, it is necessary to go for a reevaluation. A physician should promptly reevaluate a patient in the event of development of health issues like:
- Severe chills and shaking (rigors)
- High fever
- Coughing up more phlegm
- Respiratory shortness (shortness of breath)
Prognosis Prevention
Treating the bacterial infections of the respiratory system in the early stages can prevent the development of this disorder. Timely diagnosis and treatment with the aid of anti-inflammatory drugs can help you prevent acute Pleuritic chest pain. However, it must be remembered that most cases of Pleuritis result from infection and are therefore unavoidable. Patients should avoid exercising too hard or exerting themselves too much which can cause them to breathe hard and worsen the pain and the condition in general.
It is necessary to contact your doctor and seek immediate medical treatment if you are suffering from high fever, respiratory shortness or sudden, acute chest pain. Early diagnosis and treatment will help you get away with little complications by curing the condition in time, thus ensuring a faster and smoother recovery for you.
References:
Celli BR. Diseases of the diaphragm, chest wall, pleura, and mediastinum. In: Goldman L, Ausiello D, eds. Cecil Medicine. 23rd ed. Philadelphia, Pa: Saunders Elsevier; 2007:chap 100.
Lee-Chiong T, Gebhart GF, Matthay RA. Chest pain. In: Mason RJ, Broaddus VC, Martin TR, et al, eds. Murray and Nadel’s Textbook of Respiratory Medicine. 5th ed. Philadelphia, Pa: Saunders Elsevier; 2010:chap 30.