What is Ependymoma?
Page Contents
Ependymomas are rare type of tumors or gliomas that develop from ependymal cells that line the ventricles as well as from central canal of spinal cord. They can develop in the spine and also in the intracranial areas. In children, these gliomas generally develop in the cerebellum. Intracranial ependymomas commonly develop in the fourth ventricle. In some rare cases, they can also occur in pelvic cavity.
Ependymoma Epidemiology
Ependymomas comprise of nearly 5 to 10% of all pediatric brain tumors and they are known to affect both boys and girls equally. The average age of patients during the time of diagnosis is around 5 years. Around 25 to 40% sufferers are below 2 years of age. Pediatric cases mostly occur in the fourth ventricle around the posterior fossa. Ependymoma accounts for almost 25% of all cases of spinal cord tumors. It also constitutes nearly 5% of all adult intracranial gliomas. Nearly 85% of all ependymoma cases are of benign myxopapillary ependymomas. The condition is sometimes associated with syringomyelia and neurofibromatosis type II.
Ependymoma Causes
The exact factors that lead to the development of these tumors are unknown at the present moment. Research is currently being conducted to determine the possible causes of ependymoma tumors.
Ependymoma Grades
Grading of the ependymoma tumors is done by observing their appearance under a microscope. This can help to understand the rate of their progression. The tumors have been graded into 3 types. The Grade 1 tumors are generally slow-developing, whereas the Grade 3 ones grow more rapidly.
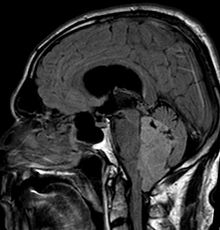
Picture 1 – Ependymoma
Grade 1
It includes Myxopapillary ependymoma, Sub-ependymoma and Sub-ependymal giant cell astrocytoma.
Grade 2
It involves low-grade Ependymoma.
Grade 3
It includes Malignant or anaplastic ependymoma and Ependymoblastoma.
Ependymoma Types
There are numerous types of Ependymoma tumors that may develop on various parts of the cranium or the spinal cord. These include:
- Myxopapillary ependymoma (MPE) – These develop mostly in the conus medullaris and the filum terminale of the spinal cord.
- Sub-ependymoma – These generally occur in fourth ventricle but may also develop in the cervical spinal cord and the septum pellucidum
- Classic ependymomas
- Sub-ependymal giant cell astrocytoma
- Anaplastic ependymoma – These usually occur in the posterior fossa.
- Ependymoblastoma – These generally develop within the supratentorial compartment.
- Extraspinal ependymoma or extradural ependymoma
- Tanycytic ependymoma – These affect the spinal cord.
- Intramedullary ependymoma – These occur in the spinal cord.
Ependymoma Morphology
These lumps are characterized by the growth of cells having regular round to oval-shaped nuclei. A fibrillary background with variable density can be seen. The tumor cells may develop gland-like elongated or round structures that look like embryologic ependymal canal having long, delicate processes that extend into the lumen. The perivascular pseudorosettes that occur frequently have the tumor cells arranged around the vessels having an intervening zone that consists of thin ependymal processes that are directed toward the walls of the vessel. The ependymomas might have originated from the radial glia.
They are found to develop in various parts of the intracranial region, as well as the spinal cord, such as:
- Posterior fossa
- Supratentorium
- Fourth ventricle
- Septum pellucidum
- Cervical spinal cord
Ependymoma Symptoms
Ependymomas are generally slow-growing tumors and their characteristic signs and symptoms may take several months to become apparent. The symptoms tend to depend on the area of the cranium or the spinal cord that is affected. The various signs and symptoms that are commonly associated with these brain tumors include:
- Sciatica
- Nausea
- Seizures
- Scoliosis
- Paralysis
- Vomiting
- Dysphagia
- Drowsiness
- Hemiparesis
- Loss of appetite
- Lower back pain
- Severe headache
- Speech problems
- Memory problems
- Difficulty in sleeping
- Bilateral Babinski sign
- Temporary visual loss
- Weakness of the limbs
- Uncontrollable twitching
- Temporary loss of memory
- Stiffness or pain in the neck
- Inadequate bladder control
- Raised intracranial pressure
- Problems with coordination
- Development of hydrocephalus
- Nystagmus or jerky eye movements
- Obstruction in the flow of the cerebrospinal fluid
- Temporary inability to identify or distinguish various colors
- Seeing horizontal or vertical lines under the presence of bright light
Ependymoma Diagnosis
While diagnosing these tumors, a doctor is likely to first conduct a thorough physical examination to check the reflexes as well as the strength arms and legs of a patient. He or she will then check for any eye symptoms that are commonly associated with this condition. Following a detailed ophthalmic examination, the doctor would also conduct the following medical tests to check the growth of tumors:
- Biopsies
- CT scans
- MRI scans
- Lumbar puncture tests
Ependymoma Differential Diagnosis
There are certain other health conditions which show signs and symptoms similar to that of Ependymoma tumors. Hence, while conducting the diagnosis, a doctor or a diagnostician needs to differentiate it from these similar-appearing conditions in order to choose the best possible mode of treatment. The differential diagnoses for Ependymoma includes ensuring the absence of conditions such as:
- Astrocytomas
- Glioblastoma Multiforme
- Choroid Plexus Papilloma
- Arteriovenous Malformations
- Tumorous growths of the conus medullaris and the cauda equina
Ependymoma Treatment
A number of treatment methods are used to manage these tumors. While deciding on the optimal method of treatment, a doctor keeps in mind the following considerations:
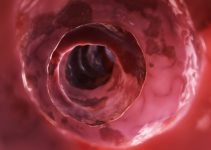
Picture 2 – Ependymoma Image
- Type, size and location of the tumor
- The extent of the disease’s progression
- The patient’s medical history, age as well as overall health
- Expected nature of progression
- Tolerance level for certain procedures, medications or therapies
- Preference and judgment of the patient’s immediate family
Surgery
Surgery is the most common form of treatment for this disorder, and is generally performed first to get rid of tumor as much as possible. The procedure is supervised by a neurosurgeon. Although complete removal of the tumor is the prime goal of the surgery, the tumor’s location or other features may sometimes make it difficult for the medical team to remove it completely.
VP shunt or Endoscopic Third Ventriculostomy (ETV)
If a tumor leads to the blockage of the cerebrospinal fluid (CSF) flow, a team of surgeons might opt for either of the two procedures to relieve signs of hydrocephalus, or build-up of fluid within the skull. A tube known as Ventriculo-peritoneal shunt (VP shunt) might be used to drain excess cerebrospinal fluid into the patient’s abdomen. Alternatively, the same might be achieved by endoscopic third ventriculostomy. In this process, the neurosurgeons create a tiny hole or an incision that allows the fluid to move past the blockage and flow into the patient’s spinal column. Almost 90% cases of pediatric ependymoma are treated in this method.
Radiation Therapy
Precise doses of radiation therapy are targeted to kill the cancer cells that are left behind even after surgical treatment. Radiation therapy is used to check the local metastasis of the tumor. Spreading of an Ependymoma might make it necessary for a doctor to recommend radiation for the whole brain and the spinal cord.
Chemotherapy
Chemotherapy effectively reduces the potential of cancer cells to spread or reproduce. Chemotherapeutic procedures prior to surgery might help to minimize the size of the tumor thereby facilitating its surgical removal. Chemotherapy drugs may be administered orally, intramuscularly, intravenously or intrathecally.
Medications
Medications might be recommended for controlling of seizures.
Ependymoma Prognosis
The outcome of the condition depends on the extent of the tumor resection as well as the age of patients. In some cases, however, the location of the tumor as well as its microscopic characteristics might also influence the overall outcome of the condition. Prognosis is good with total resection of the tumor. Instances of recurrences have been recorded in cases where total resection was not possible. A residual tumor is also most likely to spread through cerebrospinal fluid, which might lead to tumor-related complications. Patients younger than 4 years of age generally have a poorer outcome due to increased incidence of lateral posterior fossa tumor growth.
Ependymoma Survival Rate
The 5-year rate of survival for adult ependymoma patients is around 50% to 55%. Survival rate for children with posterior fossa tumors is significantly less.
Ependymomas are ependyma-related tumors that develop in the spinal cord or cranium. They can cause pressure within the cranium which can cause several complicated symptoms. Treatment needs to be followed up by regular medical checkups for several years to check for any signs of tumor recurrence.
References:
http://www.childrenshospital.org/az/Site841/mainpageS841P0.html
http://www.childhoodbraintumor.org/brain-tumor-types-and-imaging/98-ependymomas.html
http://www.braintumor.org/patients-family-friends/about-brain-tumors/tumor-types/Ependymoma.html