What is Eagle Syndrome
Page Contents
Eagle syndrome, also called Eagle’s syndrome, styloid syndrome, stylohyoid syndrome, styloid-carotid artery syndrome, and styloid-stylohyoid syndrome, refers to a health condition that causes sharp pain in the face, neck, and back of the throat. The rare condition, named after Dr. Watt Eagle, occurs due to calcified (ossified) stylohyoid ligaments (CSL) and elongated styloid processes (ESP) that exert pressure in the neck and head thereby affecting the cranial nerves.
What causes Eagle Syndrome
Although the causes of ESP and CSL are not well understood, chronic renal failure and abnormal calcium-phosphorous metabolism might be associated with their occurrences.
Eagle syndrome can be categorized into two types depending on whether it is occurring due to an ESP or CSL:
- Classic Eagle syndrome: It commonly occurs after tonsillectomy due to cranial nerve compression, resulting in inflammation and ossification of the stylohyoid ligament, with symptoms usually appearing on one side of the head and neck (unilateral). But can affect both sides (bilateral) on rare occasions.
- Vascular Eagle syndrome: Elongation of styloid processes, caused by their angulation in the middle or at the end, leads to an impingement of carotid artery wherein turning the head might compress it or tear the blood vessel.
Signs and Symptoms
Classic Eagle Syndrome
- Sharp pain in the face and neck, radiating to ears, jaw, base of the tongue, throat, or chest
- Difficulty in swallowing (dysphagia)
- Change in voice
- A lumpy feeling in the throat
- Earache (otalgia) or ringing noise in the ear (tinnitus)
- Hypersalivation
- Vertigo or dizziness
Vascular Eagle Syndrome
- Loss of consciousness due to a fall in blood pressure (syncope)
- Sympathetic plexus irritation, where irritation of certain network of veins and nerves close to the neck and head leads to feeling of discomfort in the eyes and abdominal pain
Complications
- Carotid dissection
- Restriction in blood flow to tissues
- Transient ischemic attack or “mini stroke,” which may increase the risks of a life-threatening stroke in the future
Diagnosis and Tests
On careful physical examination, palpation of the tip of styloid processes triggers pain and makes the symptoms worse, which is not possible if the styloid processes are of normal length (approximately 2.5 cm). Application of a local anesthetic to the tonsillar sinus can help with the diagnosis as lessening of the pain following the injection may suggest eagle syndrome.
Imaging Tests
- Cervical spine radiology (X-rays)
- CT scanning with three-dimensional (3D) reconstruction of the neck and skull base
Differential Diagnosis
- Glossopharyngeal neuralgia
- Laryngopharyngeal dysesthesia
- Esophageal diverticula
- Sluder syndrome
- Migraine-type headaches
- Hyoid bursitis
- Trigeminal neuralgia
- Toothache or temporomandibular disorders
- Glossodynia
- Cervical arthritis
- Otitis
- Impacted/unerupted molar teeth
- Temporal arteritis
- Faulty dental prostheses
- Cervical mass
- Carotid artery dissection
- Possible tumors
- Salivary gland disease
- Sphenopalatine neuralgia
- Fibromyalgia syndrome
Treatment and Management
Initial treatment involves conservative methods like use of oral medications and local anesthetics.
Medical Therapy
The following medications may be used for treating or lessening the symptoms of Eagle Syndrome:
- Antidepressants (amitriptyline, tianeptine) and anticonvulsants (gabapentin, pregabalin) affect neurotransmitters and lessen nerve stimulation, thereby providing relief from pain.
- Analgesics (acetaminophen, tramadol) are used for reducing pain.
- Local infiltrative administration of steroids or anesthetics like lidocaine induces numbness in the area.
Surgery
When patients do not respond to medications, surgical procedures such as styloidectomy are carried out to remove the elongated part of the styloid.
Intraoral (transpharyngeal) Approach: The elongated styloid process is detected through external examination so it can be cut out through a small incision in the muscles. It is a short, minimally invasive surgery that does not lead to any permanent scarring. But, this approach is associated with a risk of blood vessel injuries and deep neck space infections as it does not give a clear representation of the internal organs during surgery.
Patients need to take only soft foods 4 to 6 hours after the operation, while they are usually discharged within 8 to 24 hours.
Extraoral Approach: It involves making an incision around the upper third of the edge of the sternocleidomastoid neck muscle, and hyoid bone. The cervical fascia and platysma muscle are cut to reach the neurovascular bundle in the neck and digastric jaw muscles, after which the styloid process is examined. Styloidectomy is done once the muscle insertions and layers of broad tendons (aponeurosis) are set apart from the styloid.
External surgical excision has a success rate of 93.4%, where most patients are discharged within 36 hours of the surgery. However, the recovery time for the extraoral technique is longer than the intraoral approach.
Follow-up Treatment
Patients are recommended to have analgesics and antibiotics for a week after surgery. Follow-up care for at least a year is crucial for recovering from styloidectomy. During this period the patient is physically examined and tested every 3 months.
Other Methods of Management
- Homeopathic medications
- Therapeutic exercises and physical therapy to relax muscles and reduce pain
- Chiropractic treatment by a licensed practitioner
Prognosis
The medical and surgical treatment methods together have a success rate of approximately 80%. However, effectiveness of a certain treatment depends on the presence of any other associated condition or causative factor.
Incidence and Prevalence
An ESP may occur in 4% of the population, out of which only 4-10.3% of the people exhibit pain and other symptoms. Therefore, the actual incidence of Eagle Syndrome is 0.16%, with the ratio between affected females and males being 3:1. People between 30 and 50 years of age are more likely to have this condition.


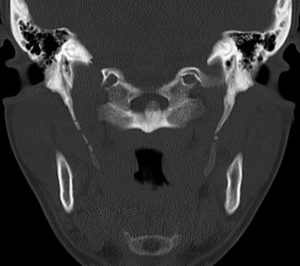
![[3] Verknoechertes Lig stylohyoideum - CT 3D - Eagle syndrome](https://www.primehealthchannel.com/wp-content/uploads/2017/04/640px-Verknoechertes_Lig_stylohyoideum_-_CT_3D-300x210.jpg)