In Thailand and Laos, Brugada Syndrome is one of the most common causes of sudden death in young males without any underlying cardiac ailments. Find out more about the fatal condition including its symptoms, causes, diagnosis and treatment.
Brugada Syndrome Definition
Page Contents
- 1 Brugada Syndrome Definition
- 2 Brugada Syndrome History
- 3 Brugada Syndrome Incidence
- 4 Brugada Syndrome Symptoms
- 5 Brugada Syndrome Causes
- 6 Brugada Syndrome Pathophysiology
- 7 Brugada Syndrome Diagnosis
- 8 Brugada Syndrome Differential Diagnosis
- 9 Brugada Syndrome Treatment
- 10 Brugada Syndrome Prevention
- 11 Brugada Syndrome Prognosis
It is a serious condition of the heart marked by abnormal rhythm that may result in sudden cardiac failure. The problem stems from the ventricles of the heart where an uncoordinated electrical activity takes place.
Brugada Syndrome History
In the 1980’s, a high incidence of unexpected cardiac failure in Asian immigrants was reported by the Centers for Disease Control. In 1989, there were few reports of this condition in patients who had survived from a cardiac arrest. However, the life-threatening disease was discovered by the Spanish/Belgian cardiologists Pedro Brugada and Josep Brugada when it led to a spontaneous cardiac death due to an impaired contraction of the ventricles in the heart.
Brugada Syndrome Incidence
It is highly prevalent in Asia, particularly in Southeast Asia. Although not a gender specific condition, it is more common in males than females between the ages of 30 and 40. According to the National Institute of Health, 5 in 10,000 people are known to be affected with the syndrome.
Brugada Syndrome Symptoms
Patients are often unaware of the condition of their heart as the disorder does not exhibit any specific symptoms. However, affected individuals may have episodes of fainting, palpitations, difficulty breathing and irregular heartbeats. These clinical manifestations are more apparent during sleep. Discomfort or pain in the chest is a sign of a sudden cardiac arrest that requires emergency medical aid.
Brugada Syndrome Causes
The abnormal cardiac disorder has an underlying genetic cause. The main function of the heart is to supply blood and nutrients to the body. The pumping of blood throughout the body is due to the regular beating and contraction of the heart. Electrical impulses traveling through the heart at regular intervals controls the heartbeat. In the upper region of the right atrium, a specialized bundle of neurons called sinoatrial node (SAN) functions as the heart’s natural pacemaker. It ensures that the blood is constantly supplied to the various regions of the body.
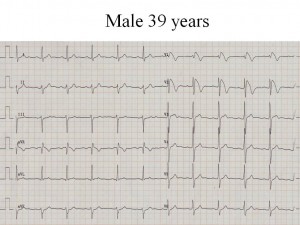
Picture 1 – Brugada Syndrome
In situations where the body demands for more oxygen-laden blood, SAN immediately increases the heart rate for greater supply. Electrical signals from the SAN get transmitted to the atrioventricular node (AVN) through special tiny pores in the cardiac muscle cells called myocetes. There is a slight delay in conduction in order to permit the atria to undergo contraction and fill the ventricles with blood. Ventricular contraction is possible only when the lower chambers of heart are completely filled with blood.
Normally, the heart beats 60-100 times a minute and this particular state is called normal sinus rhythm. However, in this syndrome, the electrical impulses arise from the ventricles in a rapid and disordered sequence. Lack of coordination between the atria and ventricles makes the heart incapable of pumping blood, resulting in fainting or sudden cardiac death depending on the severity of the disorder. Medically, this condition is known as ventricular fibrillation. Health experts believe that there is a defect in the tiny pores of the muscle cells in the right atrium that restricts the normal movement of sodium through them.
In some cases, the syndrome is acquired as a side effect of some medications used for treating high blood pressure, depression and other psychological disorders. Factors such as high blood levels of calcium or potassium and abnormally low levels of potassium can trigger a cardiac failure.
Brugada Syndrome Pathophysiology
The cardiac deficit can be attributed to a defect in SCN5A gene that encodes the sodium ion channel in the cell membranes of the muscle cells of the heart. The sodium ion channels are essential for the positively charged metal ions to get transported into the cardiac muscle cells in order to maintain a normal heart rhythm. Nearly 300 mutations occur in the gene and causes alteration in the function of the channel, reducing the flow of sodium ions into the myocytes. Abnormal heart rhythm is a consequence of a defective ion transport channel. The mutated gene is located on the short arm of the third chromosome called 3p21.
In the innermost layer of the heart called pericardium, the SCN5A gene undergoes loss-of-function mutations, resulting in transmural and epicardial dispersion of repolarization. The condition is inherited in an autosomal dominant manner, which means affected parents have a 50% chance of passing the mutant gene to their children. Mutations may even occur in the GPD1L gene that contains sites homologous to the cardiac sodium channel protein encoded by the SCN5A gene, or in cardiac calcium channel encoding genes (CACNxxx). The right ventricle seems to get more affected than the left one.
Brugada Syndrome Diagnosis
Electrocardiogram (ECG) is a standard test for measuring the electrical activity of the heart. Here, electrodes are attached to the outer surface of the skin using a device placed external to the body. The disorder has a characteristic ECG pattern, which aids physicians in diagnosing it. Patterns of abnormal electric activity are definitely a cause of an irregular cardiac rhythm. Doctors may consider intravenous administration of sodium channel-blocking drugs for the heart rhythm to undergo change. This would support the ECG in detecting the condition. These medications may induce arrhythmia, an abnormal electrical activity in the heart. In addition to this procedure, physicians may order the following tests:
Electrophysiology study
The test records both electrical activity and pathways of the heart. It is an appropriate way to determine the underlying cause of the abnormal heart rhythm. The procedure is minimally invasive and comprises of several steps. Patients are not supposed to ingest or drink for up to 12 hours prior to the test as it may lead to complications. The exact site of origin of an abnormal heart rhythm can be located with this technique.
Blood test
Elevated levels of creatine kinase and troponin in the blood are the significant indicators of several cardiac disorders, including the genetic syndrome.
Genetic testing
Patients who are suspected of having the disorder can be tested for a mutation in SCN5A gene. The test is highly essential for the early identification of the defective gene in family members who are at a potential risk.
Magnetic resonance imaging
The imaging technique is generally performed to find out the cause of arrhythmia or any other form of cardiac injury.
Brugada Syndrome Differential Diagnosis
The following conditions need to be excluded while conducting the diagnosis of this cardiac syndrome:
- Pulmonary Embolism
- Hypothermia
- Acute pericarditis
Brugada Syndrome Treatment
The main aim of the treatment is to eliminate arrhythmia that leads to a fatal consequence. The heart rhythm disturbance is an unusual condition for which medications are not available. The only approach that can help in reducing the chances of a sudden cardiac death is an automatic implantable cardioverter-defibrillator (ICD). The device is basically a small battery-powered electrical impulse generator that needs to be implanted in affected patients similar to a pacemaker. ICD constantly monitors the rate as well as rhythm of the heart, and in case an arrhythmia is detected, it corrects the condition by delivering a jolt of electricity. Tachycardia or rapid heart rhythm is a precursor of ventricular fibrillation that needs to be terminated to avoid a cardiac arrest. Advanced forms of ICD are installed with several features that can prevent tachycardia from progressing to ventricular fibrillation. Implantation of an ICD may often generate shocks.
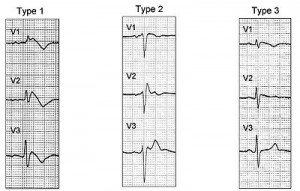
Picture 2 – Brugada Syndrome Image
Patients who may carry the risk of a coronary artery disease need to undergo angiography before an ICD implantation. Therefore, the device must be programmed in such a way that it is highly compatible with the patients. Quinidine, a class 1 anti-arrhythmia pharmacological agent, may help in preventing the development of ventricular fibrillation by increasing the duration of action potential.
Brugada Syndrome Prevention
Affected individuals must avoid taking sodium channel blockers, anti-depressants and anti-arrhythmic drugs as these agents can easily trigger ventricular fibrillation. Use of paracetamol/Tylenol can also elicit the syndrome in few patients. Any form of vigorous physical activity must be avoided to prevent any episodes of abnormal heart rate and ventricular contraction.
Brugada Syndrome Prognosis
Untreated patients normally have a poor prognosis. Asymptomatic patients could develop ventricular tachycardia within two years. ICD implantation has however, decreased the rate of mortality and shown effective results, especially in younger patients.
Brugada Syndrome is an emergency medical condition that needs to be assessed as early as possible. Genetic screening and counseling of patients as well as their family members, is recommended by most healthcare providers. Long-term monitoring of the patients post ICD implantation is highly essential.
References:
http://en.wikipedia.org/wiki/Brugada_syndrome
http://emedicine.medscape.com/article/163751-overview
http://www.mayoclinic.com/health/brugada-syndrome/DS01142
http://ghr.nlm.nih.gov/condition/brugada-syndrome