What is Bowen’s Disease
Page Contents
Bowen’s disease is a rare, slow-growing, non-hereditary skin disorder, characterized by reddish, scaly patches. Named after physician JT Bowen, who discovered it in 1912, it is also referred to as squamous cell carcinoma in situ, indicating that it is an early stage of skin cancer. However, it has been estimated that amidst 100 patches of Bowen’s disease, only three may turn cancerous.
Signs and Symptoms
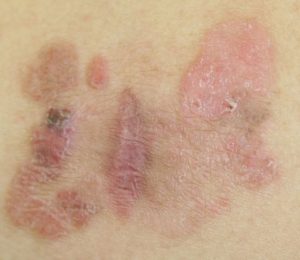
The most prominent symptom is a single scaly patch with an irregular outline, but there may be multiple patches too. There are some characteristics of these patches that help with initial detection:
Color: Reddish brown, pink or white
Size: Diameter may range from a few millimeters to several centimeters
Features: May bleed, ooze pus, itch, split open or become warty, crusted, delicate and darkly pigmented
Affected areas: Commonly affects the lower legs, arms, ears, face and neck. Less affected areas include the head, palms, anus, vulva, soles, scalp, lips as well as the area around nails and inside mouth. In young adults, the genitals are mostly affected.
Causes
The disorder occurs when the keratinocytes cells, present in the outer layer of the skin, grows abnormally fast, resulting in the flaky accumulation of dead skin cells. However, what exactly triggers such a sudden growth is not known. There are certain factors often associated with the occurrence of the disease.
Risk Factors
The disorder, more common in aged women than in men, is most likely to affect those who:
- Have a suppressed immune system due to medication or other medical ailments
- Are exposed to ultraviolet rays of the sun for long durations
- Are exposed to arsenic through food or medicine
- Have been infected with human papillomavirus (HPV)
- Are exposed to ionizing radiation
- Have a previous skin injury such as scarring
- Have inflammatory skin problems such as eczema
- Are suffering from some rare genetic disorder
Complications
- Internal malignancy
- Lung Cancer
Diagnosis and Tests
The diagnosis generally involves:
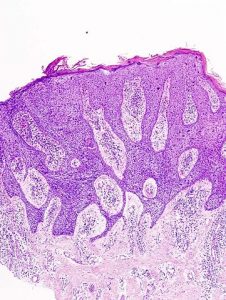
- Skin examinations to thoroughly evaluate the symptoms and rule out other skin problems
- Biopsy of the affected tissue to confirm the disease
Differential Diagnosis
- Actinic keratosis
- Basal cell carcinoma
- Squamous cell carcinoma
- Seborrhoeic keratosis
- Psoriasis
- Eczema
- Bowenoid papulosis
- Paget’s disease of the breast
- Lupus vulgaris
- Ringworm
Treatment and Management
There are different treatment measures available for this noncontiguous disorder; but first, the following factors are evaluated.
- The size and thickness of the lesion
- The number and location of the patches
- Age, general health, and ability of the affected person
Treatment Options for Small Lesions
SurgeryThis is executed by removing the affected skin patch of areas such as the genitals.
Topical Application of Creams
Chemotherapy creams such as 5-fluorouracil (5-FU) and imiquimod applied directly on the lesion, once or twice daily for about two weeks, may help in eliminating the abnormal cells, and slowing down their growth. However, both may have side effects such as redness and inflammation which may require the application of a mild steroid cream like Fucibet.
Curettage and Electrocautery
After giving a local anesthetic, the concerned patch is scraped away, and electricity or heat is then employed to stop any bleeding that occurs and to remove any existing abnormal cell. A scab that develops afterward naturally falls off within a few weeks.
Treatment Procedures for Large Lesions
Photodynamic Therapy (PDT)
A short procedure lasting for about 20‑45 minutes, it is carried out by applying a light sensitive cream on the affected area before directing a light source to activate certain chemicals in the cream, which then burn the abnormal cells. The side effects comprise of a stinging or burning sensation that goes away within a few weeks.
Cryotherapy
Done by spraying liquid nitrogen on the patches to freeze them, this procedure may leave the skin feeling cold and uncomfortable for some days. A scab that appears after a few days generally falls off, thereby removing the affected patch.
Mohs SurgeryIn this surgical excision, the edges of the lesion are traced using a microscope to remove only the cancerous tissues, while the surrounding healthy tissue is left undisturbed. Having the highest cure rate amidst all the treatment procedures mentioned here, it is usually carried out in case of large, recurrent lesions or in areas such as around the nail that need maximum preservation of its tissues.
Investigational Therapies
Radiotherapy and Laser Treatment
Laser therapy utilizes intense light to eliminate the affected tissues from small areas such as a finger. In radiotherapy, X-rays or grenz ray radiation is given if there are multiple patches to treat. However, these procedures are not widely employed and more research needs to be done to prove their effectiveness in the long run.
Can Bowen’s Disease be Prevented
It can be prevented by following appropriate measures like:
- Avoiding prolonged exposure to direct sun rays
- Always applying sunscreen when going outside
- Using safe tanning options like cosmetic bronzers
- Wearing protective clothing
Prognosis and life Expectancy
Bowen’s disease has a considerably high survival rate when taken care of properly at an early stage. However, if left untreated, it may progress to a life threatening invasive squamous cell carcinoma in 3% to 5% of patients. Hence, it is vital to have regular follow-ups with a certified dermatologist to detect signs of recurrence, which occurs in 1 out of 10 cases.
Bowen’s Disease ICD-9-CM Codes and ICD-10-CM Codes
The ICD-9-CM code of Bowen’s Disease is 230 234 and ICD-10-CM code is D04 (ILDS D04.L10)