What is Acute Lymphoblastic Leukemia?
Page Contents
- 1 What is Acute Lymphoblastic Leukemia?
- 2 Acute Lymphoblastic Leukemia Epidemiology
- 3 Acute Lymphoblastic Leukemia Causes and Risk Factors
- 4 Acute Lymphoblastic Leukemia Pathophysiology
- 5 Acute Lymphoblastic Leukemia Symptoms
- 6 Acute Lymphoblastic Leukemia Diagnosis
- 7 Acute Lymphoblastic Leukemia Differential Diagnosis
- 8 Acute Lymphoblastic Leukemia Treatment
- 9 Acute Lymphoblastic Leukemia Prognosis
- 10 Acute Lymphoblastic Leukemia Survival Rate
- 11 Acute Lymphoblastic Leukemia Diet
Acute lymphoblastic leukemia (ALL) is a type of leukemia or white blood cells cancer that is characterized by an excess of lymphoblasts. Immature and malignant white blood cells multiply continuously and are overproduced within the bone marrow. ALL leads to death and destruction of the normal cells by isolating within the bone marrow as well as by infiltrating or spreading to the other organs.
ALL may prove itself to be a fatal condition within a very short period of time if it is left untreated. The word “acute” actually refers to the short time period of the disease and allows differentiating ALL from chronic lymphocytic leukemia that may last for many years. The term Lymphoblastic is often used interchangeably with Lymphocytic. This refers to the involved cells which, although normally referred to as Lymphocytes, are found in a rather immature state in this disease.
Acute Lymphoblastic Leukemia Epidemiology
As per statistics related to the United States, the incidence of ALL is nearly 6000 new cases in every year, as of the year 2009, or close to 1 in every 50000. This form of leukemia is mostly common during one’s childhood, with peak incidence occurring between 2 to 5 years of age. Although the disease might also affect adults, prevalence among the grownups is rare, and the chances of a successful cure are greatly reduced.
Acute Lymphoblastic Leukemia Causes and Risk Factors
This form of leukemia occurs when the body generates a large count of immature WBC known as lymphocytes. The cancerous cells grow quickly and replace the normal cells that are present in bone marrow. The soft tissue present at the center of the bones is referred to as bone marrow and its function is to assist in the formation of blood cells. However, ALL prevents the manufacturing of healthy blood cells. This can give rise to life-threatening symptoms.
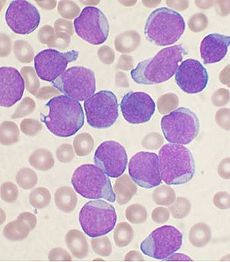
Picture 1 – Acute Lymphoblastic Leukemia
The bone marrow cells develop some errors in their DNA, due to which erroneous signals are sent to the cell for continuing cellular growth and division. This is against the norm, as a healthy cell will stop undergoing division and die. In such cases, production of blood cells becomes abnormal. Immature cells are produced by the bone marrow that progresses into the leukemic WBC known as lymphoblasts. The abnormal lymphoblasts cannot function properly and can accumulate within the healthy cells. It is however not clear as to what factors are responsible for the DNA mutations which might lead to an acute lymphocytic leukemia. Doctors are of the opinion that most cases of ALL are not inherited.
ALL is mostly seen in children aged between 3 and 7 years old, and is the most prevalent form of childhood acute leukemia. There are no obvious causes for the development of this condition in most instances. However, certain factors may aggravate the possibilities of developing leukemia on a general level. These include the following:
- Toxins, such as benzene
- Certain chromosome problems
- Bone marrow transplant
- Having a sibling with leukemia
- Exposure to x-rays and radiation before birth
- Past treatments using chemotherapeutic drugs
- Medications to suppress the immune system after an organ transplant operation
Inheritance of certain genetic disorders might aggravate the chances of a child having this disorder. These conditions include the following:
- Fanconi anemia
- Down syndrome
- Neurofibromatosis
- Ataxia telangiectasia
- Klinefelter syndrome
- Li-Fraumeni syndrome
Acute Lymphoblastic Leukemia Pathophysiology
Cancer occurs due to damage suffered by the DNA which results in an uncontrolled cellular growth as well as spreading throughout the body. This is done either by increasing the chemical signals that lead to growth or by disrupting the chemical signals that supervise growth. Development of the fusion genes can lead to the damage, as well as dysregulation of a certain proto-oncogene through its juxtaposition to the supporter of the T-cell receptor gene. Environmental factors like drugs, chemicals or radiation may be instrumental in causing this damage.
ALL is also linked with an exposure to chemicals in humans and animals as well as radiation. The connection between leukemia and radiation in humans has been clearly established in the studies done with the victims of Chernobyl nuclear reactor as well as Hiroshima and Nagasaki atomic bomb cases during World War II. Exposure to benzene or other chemicals might give rise to leukemia in animals.
Acute Lymphoblastic Leukemia Symptoms
The initial symptoms of this form of leukemia are not exactly specific to the condition but they might worsen to the extent that medical assistance is required. Lack of healthy and normal blood cells is caused by the immature and malignant leukocytes. Hence, people having this condition experience symptoms that occur due to malfunctioning of leukocytes, erythrocytes and platelets.
The symptoms and signs of acute lymphoblastic leukemia are variable. However, they generally follow bone marrow replacement or organ infiltration.
- Fever
- Anemia
- Paleness
- Vomiting
- Joint pain
- Bone pain
- Headache
- Ecchymoses
- Night sweats
- Breathlessness
- Decreased neutrophil count
- Easy bruising and/or bleeding
- Generalized fatigue and weakness
- Pain or a sensation of fullness below ribs
- Enlarged liver, lymph nodes and/or spleen
- Excessive instances of unexplained bruising
- Weight loss accompanied by a loss of appetite
- Frequent, unexplained spells of fever and infections
- Petechia; tiny red lines or spots in the skin formed as a result of low platelet levels
- Pitting edema or swelling around the lower limbs or in the abdomen (Lymphadenopathy)
Acute Lymphoblastic Leukemia Diagnosis
The diagnostic procedure for ALL begins with an examination of the medical history of a patient, which is then followed by a thorough physical examination, a complete blood count test and blood smears. The blast cells are inspected on the blood smears in the majority of cases. These blast cells are actually precursors or stem cells to every immune cell lines. The conclusive proof for acute lymphoblastic leukemia is obtained from bone marrow biopsy. A lumbar puncture or a spinal tap can confirm if the patient’s brain or spinal column has been invaded.
Cytogenetics, pathological examination and immunophenotyping help to establish whether the myeloblastic (eosinophils, neutrophils or basophils) or the lymphoblastic (T lymphocytes or B lymphocytes) cells are causing the problem. The RNA testing procedure helps to understand the intensity of the disease.
Immunohistochemical testing can reveal TdT or the CALLA antigens on leukemic cells’ surface. Medical imaging tests like CT scanning or ultrasounds can find if any other organs have been affected, namely:
- Lungs
- Spleen
- Liver
- Lymph nodes
- Kidneys
- Brain and the reproductive organs
Other diagnostic tests commonly used for this condition include:
- Biopsy
- Chest x-ray
- Cytogenetics
- Flow cytometry
- Coagulation studies
- Electrocardiography
- Bone marrow aspiration
- Gene expression profiling
- Polymerase chain reaction
- Multiple-gated acquisition scanning
- Chemistry profile, which includes lactic dehydrogenase, liver function, uric acid, and BUN/creatinine
Acute Lymphoblastic Leukemia Differential Diagnosis
While diagnosing ALL, care should be taken so as to differentiate it from certain other conditions showing similar symptoms. These include:
- Lymphoma, B-Cell
- Lymphoma, Non-Hodgkin
- Lymphoma, Mantle Cell
- Acute Myelogenous Leukemia
- Lymphoma, High-Grade Malignant Immunoblastic
Acute Lymphoblastic Leukemia Treatment
The effectiveness of the treatment of ALL depends on how early the condition is diagnosed. The aim of management is to induce lasting remission, which involves absence of any detectable cancer cells within the body.
Treatment options for acute lymphoblastic leukemia include:
- Chemotherapy
- Radiation therapy
- Steroids
- Intensive combined treatments and growth factors
Chemotherapy
This is the most used method for treating ALL. The majority of the patients are going to get a combination of various treatment methods. Due to the distribution of malignant cells throughout the body, no surgical methods for the condition have been identified yet. Generally, cytotoxic chemotherapy for this form of leukemia combines different types of antileukemic drugs. Chemotherapy for ALL is divided into 3 phases, namely:
Remission induction
This phase aims at rapidly killing most of the tumor cells to quickly get the patient into the path of remission. The target is to bring down the presence of leukemic blasts lower than 5% within the bone marrow and normal blood cells as well as ensure the absence of the tumor cells from the blood or negation of any symptoms and signs of the disorder. CNS prophylaxis should commence from this stage and continue in the next stage as well.
Consolidation/intensification
A high dosage of intravenous multi-drug chemotherapy is used to reduce the burden of tumor further.
Maintenance therapy
The main aim of this stage is to get rid of any residual cells that were not killed during the prior two phases. Although the number of such cells is minimal, they might lead to a relapse if not removed.
Radiation Therapy
This form of treatment is employed for the painful bony areas, during critical conditions, or to prepare for bone marrow transplantation. Recurrence of cerebral leukemia is prevented by using radiation therapy as whole-brain radiation for CNS prophylaxis.
Biological Therapy
Targeting protein complexes like proteasome, together with chemotherapy, has shown promising results in the clinical trials for the management of some sub-types of relapsed ALL. Selecting biological targets based on their combinatorial influence on leukemic lymphoblasts might lead to medical trials for advancement in the outcomes of ALL treatment procedures.
Immunotherapy
Modified HIV was employed for reprogramming the immune system of patients to attack the malignant cells exhibiting CD19 protein. The method has met with some initial success in experimental therapies.
Acute Lymphoblastic Leukemia Prognosis
The majority of the children or pediatric patients with ALL can be completely cured with proper treatment. Children normally have a better prognosis than the adults.
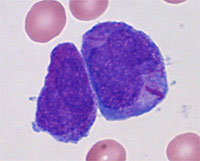
Picture 2 – Acute Lymphoblastic Leukemia Image
The following groups of patients generally tend to have a better outcome:
- Children aged between 1 and 9 years
- Younger adults, especially the ones aged below 50 years
- Those having a WBC (white blood cell) count less than 50000 during initial diagnosis
- Patients who do not undergo a specific genetic alteration known as Philadelphia chromosome-positive Acute Lymphoblastic Leukemia
- Those who experience remission only within 4 to 5 weeks of the beginning of treatment
If the leukemia spreads or metastasizes to one’s brain or the spinal cord, an affected individual is likely to have a much worse outcome.
Acute Lymphoblastic Leukemia Survival Rate
After chemotherapeutic procedure, the survival rate of the children is close to 80%. Adults, on the other hand, have a life expectancy of 40%.
Acute Lymphoblastic Leukemia Diet
Patients of ALL should follow a well-balanced, healthy diet high in nutrition and consisting of plenty of fresh fruits, vegetables, lean protein sources, whole grains, healthy fats as well as low-fat dairy foods. Individuals might be asked to follow a neutropenic diet to reduce vulnerability to probable food-borne diseases.
Acute lymphoblastic leukemia is a cancerous condition of the WBC that is characterized by an excess of lymphoblasts. The condition affects both children and adults, and the outcome of the treatment is better with younger patients.
References:
http://en.wikipedia.org/wiki/Acute_lymphoblastic_leukemia
http://www.nlm.nih.gov/medlineplus/ency/article/000541.htm
http://www.mayoclinic.com/health/acute-lymphocytic-leukemia/DS00558
http://www.webmd.com/cancer/acute-lymphoblastic-leukemia
http://emedicine.medscape.com/article/207631-overview