The post Trench Mouth appeared first on Prime Health Channel.
]]>Trench mouth is a rare bacterial infection characterized by ulcers, swelling, and inflammation of the gums. The condition got its name when soldiers in World War 1 were affected by severe gum problems as they were deprived of proper oral hygiene in the trenches.
The medical terms of this rapidly growing type of gingivitis are Vincent’s stomatitis, acute necrotizing ulcerative gingivitis (ANUG) and necrotizing ulcerative gingivitis. It is sometimes mistaken for a thrush or oral yeast infection.
Signs and Symptoms
Symptoms begin abruptly, with the earliest ones being:
- Bad breath
- Metal taste in the mouth
Other symptoms include:
Related to the Gums
- Excessive bleeding even with slight external pressure
- Gnawing pain
- Swelling
- Redness
- Development of crater-like sores between the teeth
- A covering of a grayish layer of dead tissues
Related to the Mouth
- Excess saliva production
- Pain while eating, talking or swallowing
Other Symptoms
- Uneasy feeling
- Sore throat
- Fatigue
- Mild fever
- Loss of appetite
- Lymph node swelling around neck, head and under jaw
What Causes Trench Mouth
The mouth generally contains a balance of harmless bacteria, fungi and viruses. Trench mouth occurs when bacteria grows abnormally and damages the gum tissues (gingiva).
The exact mechanism of bacterial infection is not known, but it’s assumed that certain enzymes, as well as toxins produced by the bacteria may be responsible.
Is Trench Mouth Contagious
Trench mouth is not contagious but it is a serious condition that needs immediate attention.
Risk Factors
It can occur in both adults and children, but is more likely to affect people between 15‑ 35. Developing countries with malnourishment and poor oral hygiene are also at risk. The other factors include:
- Recurring infection of tooth, mouth or throat
- Vitamin deficiencies (especially vitamins B and C)
- Emotional stress
- Smoking
- Diabetes
- Weak immune system
- HIV/AIDS
Complications
- Mouth ulcers
- Tooth loss
- Dehydration
- Gangrenous stomatitis
- Peritonitis
- Toxemia
- Vincent’s angina
How to Prevent Trench Mouth
Trench mouth is a rare ailment and can be prevented by avoiding the risk factors. Practicing some good habits like the following can help reduce the chances of developing the infection:
- Abstaining from smoking or chewing tobacco
- Practicing some stress relief techniques like yoga and exercise for minimizing stress
- Going to the dentist for a professional oral cleaning once every six months
Tests and Diagnosis
The doctor may order the following tests if trench mouth is suspected:
- A detailed clinical examination of teeth and gums
- Dental X-ray to determine the severity of the infection and to see how much tissue has been damaged
- Blood tests to find out the type of bacteria causing the damage
- Throat swab culture test for further confirmation of the condition
Differential Diagnosis
- Adrenal insufficiency and adrenal crisis
- Allergic reaction
- Fungal infection
- Blood dyscrasias
- Chronic debilitating disease
- Gingivitis diabetes mellitus
- Gingivitis, desquamative
- Gingivitis pregnancy
- Gingivitis, phenytoin
- Glossitis
- HIV/AIDS-related periodontitis
- Inadequate plaque removal
- Noma (cancrum oris)
- Pericoronitis
- Periodontitis
- Yeast
Trench Mouth Treatment
The treatment, directed at curing the infection and relieving the symptoms, is carried out on the basis of which stage the infection has reached and whether severe symptoms and complications like fever or enlargement of lymph nodes have developed.
Home Remedies to Get Rid of Trench Mouth
In the early stages of the infection, rinsing with salt water, chlorhexidine or a hydrogen peroxide solution can help in softening sore gums and in removing dead tissues. Baking soda may also be used for rinsing since it may prevent the infection from spreading.
Medication to Prevent the Infection from Spreading
In more serious cases, Antibiotics such as such as amoxicillin, erythromycin, and tetracycline can prevent the infection from spreading further, especially where a professional cleaning is not done immediately.
Professional Cleaning
For relatively mild infections with little or no complications, a thorough cleaning of the gums is achieved after three successive sittings. In the first, superficial deposits of plaque are removed by using ultrasonic scalers. In the second and third, root planning and scaling are done.
In case there are complications present, the primary cleaning procedure may also involve removal of a gray substance covering the affected gums, using a cotton dipped in hydrogen peroxide.
Medicines such as penicillin or metronidazole may also be prescribed following the cleaning, along with instructions to rinse the mouth with a 3% diluted hydrogen peroxide once every 2 hours during the healing period. If the condition of the gums gradually recovers, ultrasonic scalers are used to remove superficial deposits in later visits, while over-the-counter pain relievers like lidocaine are recommended to minimize pain.
Surgery for Severe Infection
If a pocket or abscess develops deep in a tissue, reconstructive and corrective surgeries may be necessary to open up the area and remove the dead, infected tissues.
Follow-up Measures
Once the treatment is complete, the patient needs to maintain proper oral hygiene to avoid any recurrence. Here are a few things that are commonly recommended in the follow-up treatment:
- Daily brushing
- Flossing
- Using a proper antibacterial mouthwash regularly
- Drinking lots of water
- Avoiding food irritants like hot and spicy food
- Proper nutrition with sufficient vitamin B- and C-rich foods
- Exercise and yoga to avoid stress
Prognosis
The condition can be cured with proper treatment and oral measures, but if left untreated, it may spread to tongue, cheeks, lips, and even the jaw bone, requiring major surgeries. Such severe cases may also interfere with the normal lifestyle of the affected person on a long run.
How Long Does Trench Mouth last
In most cases, the recovery time necessary is no more than a few weeks, but it is rather painful till treated.
Trench Mouth ICD-9-CM Codes and ICD-10-CM Codes
The ICD-9-CM code of Trench Mouth is 101, and ICD-10-CM code is A69.1.
The post Trench Mouth appeared first on Prime Health Channel.
]]>The post Cryptococcal Meningitis appeared first on Prime Health Channel.
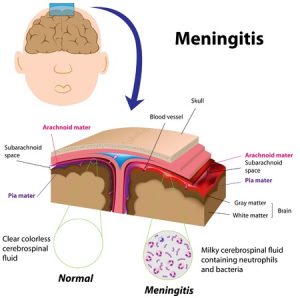
]]>Cryptococcal meningitis is a non-contagious, opportunistic infection that occurs when the meninges tissue covering the brain and spinal cord get infected by certain fungus. Other body parts, such as the lungs, kidney, bone marrow, urinary tract, lymph nodes and skin, may also be affected.
Causes
The disease is usually caused by the fungus, Cryptococcus neoformans, (present in the wastes of birds such as pigeons, as well as in soil), and rarely by Cryptococcus gatti (commonly found around eucalyptus trees). The mode of transmission of C. neoformans is through inhaling dust particles contaminated with dried bird droppings, with the fungus mostly affecting individuals having a weak immune system. The C. gatti fungus, on the other hand, may infect anyone.
Signs and Symptoms
Symptoms are slow and may take a few days to a few weeks to appear, generally including:
- Headache
- Hallucinations
- Nausea
- Vomiting
- Behavioral changes suggesting mental confusion
- Irritability to light
- Eye problems such as impaired vision
- Seizures
Rare symptoms may include:
- Moderate to high fever
- Stiffness and pain in neck
- Fatigue
Risk factors of C. neoformans-Induced CM
It is more likely to affect people with:
- CD4 cell counts below 100
- Aids
- Cirrhosis
- Diabetes
- Leukemia
- Lymphoma
- Sarcoidosis
- An organ transplant
- Long term steroid therapy
- Renal failure
- Systemic lupus erythematosus (SLE)
- After renal transplant (rarely)
Possible Complications
- Deafness
- Brain damage
- Coma
- Hydrocephalus
- Critical skull swelling leading to pressure on brain
- Blindness from optic neuritis
- Decreased mental capacity
- Meningoencephalitis
- Permanent cranial nerve palsies
- Hydrocephalous
- Vasculitis
- Ischemic stroke
Diagnosis and Tests
- A complete physical examination concerning the symptoms associated with the ailment
- A lumbar puncture test or spinal tap to examine a sample of cerebrospinal fluid (CSF)
- Chest x-ray
- CT scan of the head
- Examination of CSF to find out cell count, glucose, and protein
- CRAG test to look for cryptococcal antigen in CSF or blood
- Gram stains
- Blood culture
- Culture of CSF
- Sometimes a diagnostic test using a dye called India ink
Differential Diagnosis
- Tuberculous meningitis
- Lymphomatous meningitis
- Hyponatraemia
Treatment and Management
Medication
Antifungal medicines such as amphotericin B, along with flucytosine may be prescribed, with the dosage continuing for two or more weeks, as necessary. Close monitoring by the doctor is often necessary to check for any toxic effects on the kidney (nephrotoxicity).
Amphotericin B may be replaced by fluconazole, if spinal fluid tests (for CM) taken in two consecutive weeks show negative results. Fluconazole may be substituted with other alternative antifungal agents such as Itraconazole or Voriconazole.
Intravenous Therapy
In case of IV therapy, amphotericin B is combined with an antifungal medicine called 5-flucytosine and inserted intravenously.
Lumbar Drainage
Some patients with raised intracranial pressure may undergo a lumbar puncture to drain excess spinal fluid to reduce the opening pressure. However, more research needs to be done in this area.
Adjunctive Treatment
Glucocorticoids, such as dexamethasone, may reduce the possibility of blindness associated with the disease.
Treatment of CM during Pregnancy
For pregnant women who have CM, the usual drug of choice is amphotericin B as it is safer than the azole drugs, like fluconazole, itraconazole and ketoconazole, which may induce birth defects.
Can CM be Prevented
Although it is not possible to prevent initial exposure to the fungus, taking a few measures may help people more at risk of developing the infection. The drug, fluconazole reduce the chances of CM for those with CD4+ counts less than 50, but long-term use can have side effects, like thrush, vaginitis or candida infections since these yeast infections are resistant to fluconazole.
Incidence and Prevalence
With AIDS patients, its incidence lies between 2-7 cases per 1000 people, while amidst non-HIV-infected people, it occurs in 0.4 to 1.3 cases per 100,000 people. The ailment is more prevalent with adults and adolescents than children (found in less than 1% of all HIV-affected children).
Prognosis and Life Expectancy
Most patients improve with adequate treatment. Recurrence may be prevented by continuing the antifungal drugs. It has a mortality rate of around 10% and chiefly with those with HIV. In Sub-Saharan Africa, the death rate of AIDS patients having the disease is around 50-70%. Research is being done to develop a vaccine to prevent the ailment.
ICD-9-CM and ICD-CM-10 Codes
The ICD‑CM‑9 code of cryptococcal meningitis is 321.0, while its ICD-CM-10 code is B45.1.
The post Cryptococcal Meningitis appeared first on Prime Health Channel.
]]>The post Brucellosis appeared first on Prime Health Channel.
]]>Brucellosis Definition
It refers to an infectious disorder that arises as a result of contact with animals that carry the Brucella bacteria. It spreads from animals to humans, most frequently through cheese, pasteurized milk and other dairy products. The disease affects many wild and domestic animals as well as people who are in cloe contact with them.
The condition is also referred to by various other names, such as:
- Bang’s disease
- Cyprus fever
- Gibraltar fever
- Malta fever
- Mediterranean fever
- Rock fever
- Undulant fever
- Mediterranean gastric remittent fever
Brucellosis ICD9 Code
The ICD9 Code for this disease is 023.
Brucellosis Symptoms
The signs and symptoms of this infectious condition may arise at anytime ranging from a few days to a few months after being infected. The symptoms resemble that of flu and generally include the following:
- Chills
- Fever
- Fatigue
- Sweats
- Headache
- Weakness
- Pain in the muscles, joint and back
The problems may go away for several weeks or months before reappearing all of a sudden. The condition turns chronic in some patients and the symptoms may persist for a number of years even after treatment.
The long-term symptoms of the disease include problems like:
- Arthritis
- Fever
- Spondylitis, an inflammatory form of arthritis that affects the spine and the neighboring joints
The condition can be difficult to detect, especially in the early stages, when its symptoms resemble that of flu. Naturally it is important to visit a doctor in case of a rapidly rising fever, abnormal fatigue, muscle aches or any other problems associated with Brucellosis.
Brucellosis Epidemiology
The incidence of this condition is higher in agrarian societies. In the USA, it has a reported frequency of 0.04 in every 100,000 individuals. It is rare in inhabitants of UK although those travelling from endemic regions should always be suspected to be having it.
High-risk regions for this disorder include:
- Middle East
- Italy
- Southern France
- Portugal
- Turkey
- Greece
- Spain
- North Africa
Brucellosis Causes
As aforementioned, the condition is caused by a bacterial infection. This is a zoonotic disorder, meaning it is an animal disease that can be transmitted to human beings. The bacteria of genus Brucella is responsible for this disorder.
In humans, the condition is caused by four types of Brucella bacteria. These are:
B.melitensis
It is responsible for the majority of cases of Brucellosis and is most frequently observed in areas like Greece, Spain, India, Latin America and Persian Gulf region among others.
B.suis
It is the most common form of Brucella bacteria that is observed in the United States. It is carried by pigs and is mostly reported in the Midwest, followed by other areas like Southeast Asia and South America.
B.canis
Brucellosis due to this form of Brucella spreads from dogs and is most frequently reported in countries like North America, South America, Japan and Central Europe.
B.abortus
It is spread from cattle and is globally reported. It has been eliminated in various European nations, Israel and Japan.
The Brucella bacteria can spread from animals to humans through any of the following ways:
Consumption of contaminated or infected food
Ingestion of infected food products such as untreated milk and other dairy products (mainly unpasteurized cheese), liver or raw meat can lead to a development of this disease.
Inhalation of aerosols
This is the most common mode of transmission in endemic regions and affects herdsmen, farmers, abattoir workers, lab technicians and families that share habitation with animals.
Skin or mucous membrane contact
Vets, lab technicians and hunters are some of the individuals who are commonly infected through this mode of transmission.
Person to person transmission
This can occur through breast-feeding, bone marrow transplantation, blood transfusion or sexual transmission. However, this type of transmission from one human to another is rare.
The bacteria responsible for this disease can also be spread through bioterrorism although Brucella is less likely to be chosen as an infectious agent due to the low mortality rate associated with it.
A form of the condition has also been found to affect porpoises, some whales and harbor seals. Coming in close contact with such types of marine infected animals can also make a person develop this disorder.
Brucellosis Risk Factors
The risk factors for this condition include:
Living in high-risk areas
Although Brucellosis is rare in the U.S, it is prevalent in various regions of the world such as areas around the Mediterranean Sea, close to the Persian Gulf, in Latin America and on the Indian subcontinent. Those who live in or travel to these regions are more likely to ingest village cheese, which is another name for unpasteurized goat cheese. This type of cheese, imported from Mexico, has also been linked to a number of cases of Brucellosis in the U.S.
Being engaged in high-risk professions
Those who are engaged in occupations that need them to come in close contact with animals or their infected blood are more susceptible to this disorder. Such people include:
- Dairy farmers
- Vets
- Lab technicians
- Microbiologists
- Ranchers
- Slaughterhouse workers
Brucellosis Diagnosis
The presence of this disorder is usually confirmed by physicians by testing a sample of bone marrow or blood, in order to determine the presence of the Brucella bacteria or for bacterial antibodies. Some additional tests may be deemed as necessary to help sufferers detect complications related with Brucellosis. These include:
X-rays
These imaging exams are useful as they can show any changes in the bones and joints of the body of sufferers.
Magnetic Resonance Imaging (MRI) or Computerized tomography (CT) scans
These exams help detect abscesses or swelling in the brain or other tissues.
Cerebrospinal fluid culture
It helps analyze a small sample of the fluid surrounding the brain and spinal cord to determine the presence of infections such as Encephalitis and Meningitis.
Echocardiography
This exam makes use of audio waves to produce images of the heart and look for signs or damages of infections in the heart.
Other assistive tests for this disease may involve:
- Bone marrow culture
- Clean catch urine culture
- Serology for brucellosis antigen
The disorder may also change the results of the following exams:
- Febrile/cold agglutinins
- Serum immunoelectrophoresis
- Quantitative immunoglobulins (nephelometry)
Brucellosis Differential Diagnosis
As the signs and symptoms of Brucellosis are non-specific in nature, they tend to be confused with those of many other disorders and agents. These include:
- Bronchitis
- Tuberculosis
- Endocarditis
- Pneumonia
- Subarachnoid haemorrhage
- Gastroenteritis
- Osteomyelitis
- Meningitis
- Thrombocytopenic purpura
- Urinary tract infection (UTI)
- Biological warfare agents
- Mechanical back pain
Physicians in charge of diagnosis must ensure that patients are not suffering from any of the above disorders and are in fact, having symptoms related with Brucellosis.
Brucellosis Treatment
In case of this disease, medical treatment has a three-fold aim:
- To bring about relief from the discomforting symptoms
- To prevent a relapse of the disorder
- To prevent complications associated with this condition
Patients need to follow a course of antibiotic medications for a minimum period of six weeks as the symptoms may not completely resolve for several months. Antibiotics can cure the infection and also prevent the recurrence of the disease.
The condition may recur and even turn chronic in some cases. Longer courses of therapy may be required in case of complications.
Brucellosis Prognosis
The condition may relapse and the symptoms may persist for several years. As is the case with tuberculosis (TB), the disorder may recur after a long span of time. The majority of sufferers manage to have a complete recovery without complications, if they get appropriate antibiotic treatment.
The rate of relapse associated with this disease is around 10%, even with proper medical treatment. Death is rare, with an approximate mortality rate of 2%, and is generally related with Endocarditis.
Brucellosis Complications
The disorder can affect about any part of the human body, including the heart, liver, reproductive system and central nervous system. Chronic cases of Brucellosis may give rise to complications throughout the body or in only one organ.
The possible complications include the following:
Arthritis
Osteoarthritis and Spondylitis are two main arthritic complications associated with this disease. The former is characterized by stiffness, inflammation and pain in the joints, particularly in the ankles, spine, wrists, hips and knees. The latter is marked by swelling of the vertebral joints and can be specifically difficult to cure; it may result in lasting damage.
Central Nervous System (CNS) Infections
CNS infections include conditions like Meningitis and Encephalitis that can bring about the death of sufferers.
Endocarditis
It is one of the most acute complications of Brucellosis. Untreated cases of this disorder can destroy or damage the cardiac valves; it is the primary cause of deaths associated with Brucellosis.
Brucellosis Prevention
The risk of acquiring this disease can be prevented by adapting the following preventive measures:
Wearing gloves while handling animals
Farmers, hunters, vets, slaughterhouse workers and other people who have to work with animals or their body should wear gloves while handling dead or infected animals or their tissue or while assisting animals at the time of giving birth.
Vaccinating domestic animals
Vaccinating domestic animals can reduce the risk of infection in them. An aggressive vaccination program in the U.S has been successful in almost wiping out Brucellosis in livestock herds.
Cooking meat thoroughly
Cooking meat of all domesticated animals at 145-165 F (63-74 C) is necessary before consumption. High heat is able to destroy all traces of bacteria present in meat products and make them safe to be eaten.
If you or any of your family members start showing one or more of the health problems associated to Brucellosis, get medical help on an immediate basis. Prompt diagnosis and treatment can keep the disease in check and prevent the occurrence of any possible complications in future. Timely cure can also ensure an early recovery from this discomforting disease.
References:
http://www.nlm.nih.gov/medlineplus/ency/article/000597.htm
http://www.mayoclinic.com/health/brucellosis/DS00837
http://emedicine.medscape.com/article/213430-overview
http://www.webmd.com/a-to-z-guides/brucellosis-symptoms-treatment
The post Brucellosis appeared first on Prime Health Channel.
]]>The post Bubonic plague appeared first on Prime Health Channel.
]]>Bubonic plague Definition
It is a zoonotic disease that is caused when a person is infected by a type of bactetium known as the “Yersinia pestis.” It is characterized by inflamed lymph nodes, historically referred to as “buboes.”
This is believed to be a disease that existed some time in history. However, the condition exists even today. It is known by various other names, like:
- Black plague
- La Peste
- Black Death
- Pestilential fever
This is among the three major types of plague, the other two being Pneumonic plague and Septicemic plague. Out of the three, Bubonic plague is the most common.
Bubonic plague ICD9 Code
The ICD9 code for this disorder is 020.0.
Bubonic plague Incidence
According to the World Health Organization, there are annually approximately 3,000 cases of this condition around the world. Around 10 to 20 of these cases occur in the U.S, most frequently in the rural regions of the Southwest.
Bubonic plague Symptoms
The signs and symptoms of this form of plague occur within 2-6 days of being infected by Yersinia pestis, the bacteria that is causative of this condition. The period between getting infected and the manifestation of symptoms is referred to as the “Bubonic plague incubation period.”
If left without treatment, patients may experience symptoms like:
- Diarrhea
- Vomiting
- Abdominal pain
The symptoms can rapidly progress to Septicemic plague, another major type of plague. Around 10-20% of all sufferers of Bubonic plague also tend to develop symptoms in the lungs. This is known as Pneumonic plague, a condition that is often life-threatening in nature.
The signs of this plague are categorized into two stages:
Early stage symptoms
These characterize the initial days after being infected with Yersinia pestis and include problems like:
- Chills
- Fever
- Headache
- Vomiting
- Nausea
- Abdominal pain
- Reduced appetite
- Diarrhea (possible bloody in nature)
- Tiny broken blood vessels (known as Petechiae)
The condition is also manifested by the development of Buboes, which are enlarged, tender lymph nodes in the neck, in the groin or under the armpits. The size of these nodes range from 1-10 cm in size and can be observed in 70% of all sufferers.
Later stage symptoms
In the later stages, the symptoms can progress to Septicemia plague on a rapid basis. The signs of this stage include the following:
- Fever
- Chills
- Severe headache
- Nausea
- Vomiting
- Rapid heart rate
- Delirium
- Death
The Bubonic plague severely affects the lymphatic system and the lungs. When it affects the lungs in 10-20% sufferers (Pneumonic plague), the symptoms include:
- Fever
- Cough
- Respiratory difficulties
- Increased breathing
- Respiratory failure
- Coughing up of blood
- Acute Respiratory Distress Syndrome (ARDS)
In such cases, death usually occurs within 1-6 days. When bubonic plague reaches the lungs, there is approximately 75% mortality rate in spite of use of proper treatment measures. The condition reaches too severe a stage to be medically treated.
In less than 10% patients, there can be development of plague meningitis. Its symptoms include:
- Fever
- Headache
- Stiff neck
- Confusion
- Coma
Bubonic plague Causes
As already mentioned, the condition arises due to infection by a bacterium known as Yersinia pestis. The bacterium is generally spread through the bites of rodents or infected fleas. However, the bacteria can also be carried by other animals like lice, chipmunks and prairie dogs. Other animals that are known to be carriers of this bacterium include:
- Cats
- Dogs
- Mice
- Wood rats
- Squirrels
Yersinia pestis is also responsible for the occurrence of two other forms of plague, Septicemic plague and Pneumonic plague. This Gram-negative bacterium can be found in various parts of the world, such as South America, Africa and Asia.
Is Bubonic plague Contagious?
This is a zoonotic disorder, which means it can be transmitted to animals from humans. This happens most often through direct contact with tissues of infected animals or through the bites of fleas.
Bubonic plague Risk Factors
The risk factors of this disorder include:
Living in susceptible regions
Residing in or traveling to areas that have a prevalence of this disease can increase the risk of development of Bubonic plague. These regions include Asia, rural regions of Southwest U.S and Africa where fleas, mice and other carrier animals of the Yersinia pestis bacterium are present.
Having close contact with infected beings
Tending to humans and animals infected with this plague and not washing hands before meals after care can greatly increase the risk of catching this contagious disorder.
Weak immunity
People suffering from weakened immunity due to the presence of conditions such as diabetes or HIV/AIDS may also be vulnerable to the Yersinia pestis bacterium that causes Bubonic plague.
Bubonic plague Diagnosis
The diagnosis of this disease begins with a physical examination of sufferers. At the time of a physical test, doctors listen to the sounds of the lungs and take a look at the appearance of the skin to check for signs of plague. Patients are asked questions about their medical history, recent exposure to some animals, history of travelling to susceptible regions and more.
If doctors suspect a possible occurrence of plague, they may recommend some diagnostic tests involving examination of lymph node fluid and samples of sputum or blood of sufferers.
The diagnosis of Bubonic plague is often confirmed by microscopic observation of a blood sample of sufferers for presence of Yersinis pestis.
Bubonic plague Differential Diagnosis
During differential diagnosis, physicians should ensure that patients are actually suffering from the symptoms of Bubonic plague and not any other condition that gives rise to similar symptoms, such as Septicemic plague or Pneumonic plague.
Bubonic plague Treatment
When a person is suspected of suffering from this form of plague, he or she is often hospitalized and kept in isolation. Medical treatment is usually initiated as early as possible, even before lab results are obtained. Treatment is usually carried out with the aid of antibiotics. Streptomycin and Gentamycin are two of the antibiotic drugs that are used for curing Bubonic plague. Chloramphenicol and Tetracyclines can also yield effective results.
Anyone having close contact with patients of this condition should be detected and assessed for presence of the microbes that are responsible for the disease. Such people should be kept under observation or administered antibiotic therapy, based on the severity of the plague and timing of exposure to the agent of infection.
In 85% of cases of this disease, early treatment for this form of plague offers a cure for the condition. The ideal plan to avoid this disease is to prevent infections in the first place. This is due to the fact that the plague vaccine is no longer available in the U.S commercially. Naturally, the treatment for this plague has three aims:
- Preventive drug therapy
- Environmental management
- Public health education
Only in 10-15% cases, the human body has been found to be able to effectively combat the Yersinia pestis bacterium that causes the Bubonic plague.
Bubonic plague Prognosis
If the condition is left without being cured, it can worsen into Septicemic plague with a 40% death rate. If not treated within 24 hours, it can get even more advanced and patients may suffer from Pneumonic plague which carries a 100% death rate.
Bubonic plague Mortality Rate
The rate of mortality is 15% if medical treatment for this form of plague if treatment is administered on an early basis. However, the mortality rate ranges from 50 to 90% if it is left untreated. In the absence of cure, the causative bacteria can quickly spread to the lungs or multiply in the bloodstream.
Bubonic plague Complications
The common complications of this disease include:
- Meningitis
- Gangrene
- Inflammation of the brain
- Decaying of tissue and bleeding
- Inflammation around the heart
- Septic shock, which can result in a blood infection
- Death, in cases that are left without being treated
Untreated cases of this form of plague have a high mortality rate.
Bubonic plague Prevention
No effective vaccines are yet available for this disorder. Scientists are still trying to develop a powerful vaccine for sufferers of Bubonic plague. If an individual has been exposed to plague or is at a risk of this disease, antibiotics can help prevent the infection.
Adapting the following measures can help void the disease in regions where outbreaks of plague occur:
Use of insect repellant
Using insect repellant is necessary in regions with huge rodent populations, where the risk of prevalence of this disease is high.
Keeping pets free of fleas
Veterinarians should be asked which flea control products work best.
Keeping homes rodent-proof
Pets and children should be closely supervised when they spend time in outdoor environments with huge rodent populations. Kids should be encouraged to use insect repellants before going out in such areas.
Bubonic plague Support Groups
Family members of individuals affected with this disease can get useful information about Bubonic plague and proper guidance from the following organizations:
World Health Organization (WHO)
Avenue Appia 20
Geneva 27, 1211
Switzerland
Tel: + 41 22 791 21 11
Fax: + 41 22 791 31 11
Internet: http://www.who.int/en/
NIH/National Institute of Allergy and Infectious Diseases
Office of Communications and Government Relations
6610 Rockledge Drive, MSC 6612
Bethesda, MD 20892-6612
Tel: (301)496-5717
Fax: (301)402-3573
Tel: (866)284-4107
TDD: (800)877-8339
Email: [email protected]
Internet: http://www.niaid.nih.gov/
Center for Disease Control and Prevention
1600 Clifton Road NE
Atlanta, GA 30333
Tel: (404)639-3534
Tel: (800)232-4636
TDD: (888)232-6348
Email: [email protected]
Internet: http://www.cdc.gov/
Bubonic plague Pictures
The images here depict the physical appearance of people affected by this disorder.
Picture 1 – Bubonic plague
Picture 2 – Bubonic plague Image
If you suspect any of your friends or family members is suffering from Bubonic plague, get in touch with a professional healthcare provider at the earliest. This will ensure that all future complications are kept at bay and the health of patients is safeguarded. As aforesaid, this disorder involves a risk of life-threatening problems. Due to this reason, it is important to seek medical attention on an immediate basis.
References:
http://www.cdc.gov/plague/faq/
http://en.wikipedia.org/wiki/Bubonic_plague
http://www.wisegeek.com/what-is-bubonic-plague.htm
http://plague.emedtv.com/bubonic-plague/bubonic-plague-symptoms.html
The post Bubonic plague appeared first on Prime Health Channel.
]]>The post Cryptosporidiosis appeared first on Prime Health Channel.
]]>What is Cryptosporidiosis?
It is a parasitic disorder that results from an infection caused by a protozoan parasite known as Cryptosporidium – which is most commonly isolated in patients who are HIV positive and present symptoms of diarrhea.
The condition is also referred to as Crypto.
Cryptosporidiosis ICD9 Code
The ICD9 Code for this disorder is 007.4.
Cryptosporidiosis Incidence
The incidence of the disorder is not much well-defined in the United States. Around 200-300 cases of Crypto are diagnosed every year in Minnesota. Approximately 400 cases are reported annually in New York. In the past two decades, it has been recognized as one of the most common causes of waterborne conditions in the U.S. This is a rare disease and only under 3,000 cases of the condition has been reported in 2011 in England and Wales, down from around 4,000 in 2008. The disorder has a higher prevalence in developing nations that have a higher prevalence of AIDS.
The incidence of the disease peaks in children who are less than 5 years old.
Cryptosporidiosis Symptoms
Stomach cramps and watery diarrhea are the most common symptoms of this disorder. Other symptoms may include the following:
- Nausea
- Vomiting
- Loss of appetite
- Fever
- Dehydration
- Loss of weight
However, some patients of this condition may not become ill at all. They may not exhibit any symptoms and may not get sick although they carry the infection and can spread the disorder to others.
The incubation period for the parasite responsible for this disease may range from 1-12 days with an average span of 7 days. Due to this reason the initial signs of the disorder appear within 1-12 days, usually 7 days on an average, after initial exposure to the parasite which is responsible for Crypto. The signs and symptoms may appear and disappear and may last for days to weeks. Those with a weak immunity may exhibit more acute symptoms that may last for several months.
If the CD4+ cell count of sufferers is below 200, the condition is more likely to lead to diarrhea as well as other symptoms for a prolonged duration. If the CD4+ cell count is higher than 200, the ailment may not last longer than 1 to 3 weeks or a little more. However, patients may still be the carriers of the infection. This indicates that the crypto parasites may not cause the ailment but may still be living in the intestines of patients. The symptoms of Cryptosporidiosis may reappear at a later stage if the CD4+ cell count drops below 200.
Cryptosporidiosis Causes
As aforesaid, it is caused by exposure to the microscopic parasite known as Cryptosporidium. Cryptosporidium infections have been reported in humans as well as various pets, native and farm animals. Some bird, reptiles and fishes may also get affected with this parasite. There are various species of Cryptosporidium. However, only Cryptosporidium hominis and Cryptosporidium parvum are supposed to cause infection in human beings. The parasite lives in water, soil and food and also inside the intestines of people that it infects. It may also survive on surfaces that have become contaminated with waste.
This microbe is shed in the feces of infected animals and humans. Humans can become infected by this organism due to its accidental ingestion. The parasite can also spread from one person or animal to another due to skin contact or due to drinking contaminated water. Following recovery from the ailment, infected people can shed the parasite in their stool for a number of weeks.
The following activities can result in the occurrence of this disorder:
- Contact with people infected by Cryptosporidium
- Swimming in contaminated pools
- Handling infected animals or their feces to produce manure
- Drinking water contaminated by Cryptosporidium
- Intake of contaminated food (in rare cases)
As the condition is transmitted through the fecal-oral route, the possibility of its transmission is the greatest from diapered children, infected individuals with diarrhea as well as people with poor hygiene.
Cryptosporidiosis Risk Factors
Certain individuals are more susceptible to infection by Cryptosporidium more than others. This high-risk group includes:
- Travelers to developing countries
- Men indulging in same-sex physical intimacy
- Individuals working in animal farms
- Parents of children infected with Cryptosporidiosis
- People working in close contact with individuals infected with Cryptosporidiosis
- Child care workers
- Those who drink untreated water from lakes or rivers
- Swimmers who swallow even small amounts of water from swimming pool
- Kids, including diapered children , who attend day care
Those with weakened immunity are at greater risk of developing an acute form of this condition.
Cryptosporidiosis Diagnosis
This infectious disorder is detected by a microscopic examination of the stool which helps in diagnosing the parasite that is responsible for the disorder. When a doctor suspects a person with diarrheal disorder to be suffering from Cryptosporidiosis, he or she tends to order a Cryptosporidium test. As yet, most laboratories do not routinely carry out the tests that are necessary to detect this specific parasite.
A Cryptosporidium test should be specifically ordered for HIV/AIDs sufferers or other immunocompromised individuals (such as cancer or transplant patients) who are undergoing treatment for diarrhea.
Cryptosporidiosis Differential Diagnosis
The differential diagnosis of this condition involves telling its symptoms apart from a range of types of Gastroenteritis, which include:
- Amoebiasis
- Escherichia coli O157
- Campylobacter enteritis
- Giardiasis
- Salmonellosis
- Shigellosis
- Viral gastroenteritis
Cryptosporidiosis Treatment
The condition does not have any specific treatment. Most people with Cryptosporidiosis get better without any medical treatment. Pain management, maintaining electrolyte balance and rehydration can ensure management of the symptoms associated with this disorder. Routine rehydration measures are usually enough to manage this disease in healthy people.
Sometimes, if dehydration occurs, administration of intravenous fluids or oral liquids may be necessary. Temporary improvement of the symptoms may be possible with anti-diarrheal medicines which decrease bowel movements.
Cryptosporidiosis patients should get benefit by getting in touch with health care providers who can discuss their diet and provide them with nutritional counseling that can minimize the symptoms of diarrhea to the best possible extent.
Cryptosporidiosis and Medications
As of now, no medication has yet been found to cure the symptoms of this disease. However, some sufferers may show positive response to some types of antibiotics. Certain drugs, such as Paromomycin, may decrease the signs and symptoms of the disorder. New medicines for the condition are still under testing stage.
The problems of dehydration can be prevented with the aid of sports-ade drinks and oral rehydration powders.
Immune-strengthening therapies such as oral probiotics are sometimes useful resolving this condition y promoting the growth of beneficial bacteria in the intestine. People who suffer from low immunity due to the presence of underlying conditions such as diabetes or AIDS can derive benefit from such therapies.
Cryptosporidiosis Prognosis
In the majority of healthy people, diarrhea induced by this condition is generally self-limited in nature. In immunocompromised individuals, however, the diarrhea is often prolonged for more than one week or persistent for over two weeks. The disorder may be acute, chronic and also life-threatening in some cases in such individuals – along with extraintestinal manifestations.
Those with Cryptosporidiosis and AIDS tend to develop chronic symptoms more frequently. Around 10% of them have a fulminant course. The outcome is generally improved with the help of antiretroviral treatment. However, persistence of some symptoms have been reported in certain individuals. These include:
- Loose stools
- Persistent abdominal pain
- Extraintestinal sequelae, such as pain in the head, joints or eyes and fatigue or dizzy spells
Cryptosporidiosis Complications
The complications of this disorder include the following:
- Persistent diarrhea
- Worsening malnutrition
- Problems in fitness and cognitive abilities
- Respiratory tract problems in healthy children as well as AIDS patients with intestinal Cryptosporidiosis
- Conditions like Acalculous cholecystis, Pancreatitis, Sclerosing cholangitis, and papillary stenosis in immunocompromised people
Chronic cases of Cryptosporidiosis may get complicated by malnutrition and malabsorption leading to death in malnourished children and individuals with AIDS.
Cryptosporidiosis Prevention
Catching this infection can be prevented by the following measures:
- Not swimming in natural sources of water, such as creeks, dams or rivers, within a week after heavy downpour
- Avoiding swallowing water while swimming
- Not drinking untreated water from streams or lakes or using them only after boiling the water to kill Cryptosporidium
- Washing hands thoroughly with water and soap for around 10 seconds after handling infected animals or their manure or changing nappies, using the toilet or working in the garden
- Avoiding foods or drinks that may possibly be contaminated, such as tap water or raw vegetables, while travelling to developing nations
The transmission of Cryptosporidium can be avoided by measures like:
- Not sharing linen or towels for at least two weeks after the diarrhea has stopped
- Not swimming in any water source for at least two weeks after the diarrhea has stopped
- Not handling food items for at least two days after the diarrhea has stopped
Children affected with this disorder and showing symptoms of diarrhea should be kept from going to childcare, school, preschool or playgroup for at least 24 hours after the diarrhea has stopped completely. Even after diarrhea ends, those infected by the Cryptosporidium parasite may return to school or workplace but keep washing their hands after using the toilet. This is due to the fact that oocysts may continue to pass into stools for weeks even after the symptoms subside.
It must be remembered that Cryptosporidium is resistant to disinfectants like chlorine. Hence, it can persist in water even after being chemical treatment. For this reason, boiling is the most reliable technique to ensure safety of water as Cryptosporidium parasites cannot survive in very high temperatures.
Cryptosporidiosis Pictures
The following images show the appearance of Cryptosporidiosis sufferers as well as the Cryptosporidium parasite.
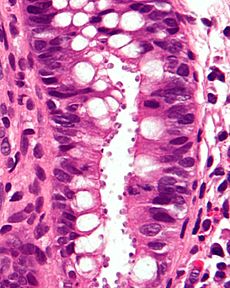
Picture 1 – Cryptosporidium Parasite
Picture 2 – Cryptosporidiosis of the colon Image
If you suspect your child, or any family member or friend, to be exhibiting the symptoms of Cryptosporidiosis, immediately get in touch with a professional medical care provider. This can ensure quick recovery from this extremely discomforting disease and also eliminate all possibilities of development of complications in future.
References:
http://en.wikipedia.org/wiki/Cryptosporidiosis
http://www.patient.co.uk/doctor/cryptosporidiosis
http://www.webmd.com/hiv-aids/prevent-cryptosporidiosis
http://emedicine.medscape.com/article/215490-overview
The post Cryptosporidiosis appeared first on Prime Health Channel.
]]>The post Toxocariasis appeared first on Prime Health Channel.
]]>Toxocariasis Definition
It is an infection caused by parasitic roundworms, medically referred to as Toxocara, which can be found in the intestines of dogs and cats. It is most common in young children who are exposed to dirt.
The disease is also referred to by various other names, such as:
- Covert toxocariasis
- Toxocara canis
- Toxocara cati
- Toxocarosis
- Ocular larva migrans
- Visceral larva migrans
The prevalence of this disorder is supposed to have a relation to geographic locations as it is found to be more prevalent in hot, humid areas where eggs are kept viable in the soil.
Toxocariasis ICD9 Code
The ICD9 Code for the disorder is 128.0.
Toxocariasis Types
The condition is classified into three types:
Covert Toxocariasis
As the name indicates, the symptoms associated to this type of the disorder are short-term and mild in nature. Patients with this form may suffer from headache, cough or mild abdominal pain. This is a mild, febrile and subclinical disease.
Visceral Toxocariasis
It arises when eggs hatch and spread all through the body, resulting in swelling of the skin, heart, lungs or even the brain. The condition is also known as Visceral larva migrans. In occasional cases, the condition has been known to give rise to pleural effusions and Chronic urticaria.
Ocular Toxocariasis
It occurs in those occasional cases when larvae spread to the eyes, causing redness and blurred vision. This form of the disease is also referred to as Ocular larva migrans. It tends to arise in older kids and young adults.
Toxocariasis Incidence
The condition has a worldwide prevalence, although most cases of it arise in places where cats and dogs are kept very near to human beings. The majority of cases are reported from regions like:
- Australia
- East and Western Europe
- Hawaii
- Mexico
- Philippines
- South Africa
- Southeastern United States
This is a rare type of infection. The Health Protection Agency (HPA) recorded only 30 cases of the disease in England and Wales between the years 2000 and 2010. The exact prevalence and incidence of this disorder is hard to determine. It is difficult to exactly assess how many cases of Toxocariasis occur every year as the disease is often undiagnosed or even misdiagnosed. It is possible that many more individuals have been exposed to such parasites without being aware.
Toxocariasis Symptoms
The majority of individuals suffering from this disorder are asymptomatic. In other words, they do not exhibit any signs and symptoms. Even if symptoms occur, they may include problems like fever, seizures and cough or wheezing.
Other symptoms may include:
- Rash
- Loss of appetite
- Abdominal pain
- Enlarged lymph nodes
- Enlarged liver or spleen
The infection can also affect the eyes and result in problems like:
- Cross-eyed appearance
- Headaches
- Reduced vision
- Inflammation around the eyes
In rare cases, the roundworm larvae can infect organs like the brain, eyes, liver or lungs and can result in acute symptoms such as:
- Fatigue
- Respiratory difficulties
- Loss of appetite
- Cloudy or blurred vision in one eye
Toxocariasis Causes
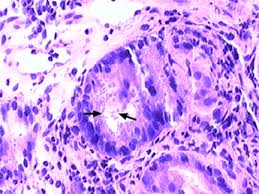
In humans, the disorder can arise as a result of migration of the larvae of Dog roundworm (Toxocara canis) and less commonly due to cat roundworm (T. cati) through the tissues of human body. Toxocara are nematode parasites of animals. Humans become infected by the microbe due to accidental ingestion of eggs in soil that is contaminated by feces of dogs. Although they never mature in human beings, larvae hatch out in the small intestine and tend to migrate through the lungs and the liver to other tissues. In the majority of cases, the larvae are possibly eliminated although a surrounding granuloma may develop in certain sufferers.
In rare circumstances, T. cati can mature in human beings and get transmitted through feces or vomit. However, sufferers with adult T. cati do not have antecedent symptoms, antibodies or eosinophilia. This indicates that they are acquired due to ingestion of adult worms or advanced larval stages from feces or cat vomit.
Toxocariasis Risk Factors
The risk factors for this disorder include the following:
- Dwelling in rural areas
- Cohabitation with cats and dogs
- Socioeconomic deprivation
- Eating without washing of hands
- Travel to regions with high prevalence of the condition
- Contact with soil contaminated with dog feces
Kids are at greatest risk of contracting this disease as they may accidentally ingest soil with contaminated eggs in playgrounds.
Toxocariasis Diagnosis
The diagnosis of the disorder can be very difficult as the majority of its symptoms are mild and nonspecific in nature. The common indicators of infection are:
- Hepatomegaly
- Chronic eosinophilia
- Chronic pulmonary disease
- History of exposure to puppies
- Contact with feces-contaminated soil
The disease is usually detected through a blood test. Blood tests look for evidence of infection with Toxocara larvae. Apart from blood test, diagnosis of the condition involves detecting the presence of typical clinical symptoms of OT or VT and knowing about history of possible exposure to dogs and cats. In order to infer diagnosis, clinicians use serologic testing such as Immunoblot or ELISA (Enzyme-linked Immunosorbent Assay).
In the majority of cases, no treatment is required. Some medicines that are useful for Toxocariasis patients may be used to remove the infection.
If a physician suspects visceral or ocular larva migrans, he or she may conduct CT scans of the inner organs to analyze the extent of damage.
Toxocariasis Differential Diagnosis
The signs of this disorder resemble those of a variety of other conditions, which adds to the difficulty of diagnosing Toxocariasis. Doctors should take all possible measures to isolate the symptoms of the condition from those of these similar diseases like:
Differential diagnosis of visceral form
This includes distinguishing the symptoms from those of the following disorders:
- Other causes of Acute hepatitis
- Angioedema
- Adverse drug reactions
- Allergic bronchopulmonary aspergillosis
- Eosinophilic pneumonia
- Hypereosinophilic syndrome
- Pulmonary eosinophilia
- Systemic lupus erythematosus
- Other helminthic infestations
Differential diagnosis of ocular form
This includes distinguishing the symptoms from those of Retinoblastoma.
Toxocariasis Treatment
The treatment for this disease is based on the form of the infection and the severity of the symptoms. Cases of Visceral Toxocariasis can be cured with the aid of antiparasitic medications like Mebendazole or Albendazole. Corticosteroids play an important role in suppressing acute allergic manifestations of the disorder.
The treatment of Ocular Toxocariasis is harder and generally involves measures to prevent progressive damage to the eye. Corticosteroids have a significant role to play even in the treatment of this form.
Most cases of covert Toxocariasis are not medically treated. The larvae are naturally expelled in bowel movements over a period of few weeks. If there is a spread of the roundworm larvae, a doctor can prescribe medications known as anthelminitics to detect and destroy parasites that are present in the bloodstream of patients. Anti-inflammatory drugs can help provide relief from other symptoms associated to infection.
In rare cases where parasites result in severe damage to eyes or organs, surgery may be required to remove or repair parts of the body that have been affected.
Toxocariasis Prognosis
Fortunately, the condition generally carries a very good prognosis. The outcome is variable in case of patients of the ocular form of the disorder. The prognosis is generally good in the visceral form. The majority of patients are found to recover without medical treatment.
Toxocariasis Complications
Uniocular visual loss is not infrequent in cases of Ocular Toxocariasis. In severe cases of Visceral Toxocariasis, prominent organ damage and even death can occur.
Toxocariasis Prevention
Controlling Toxocara infection in cats and dogs can reduce the number of infectious eggs in the surroundings and decrease the risk of infection for sufferers. Veterinarians should be hired to cure cats and dogs, particularly those of young age, to regularly check for the presence of worms. This is particularly necessary in cases where pets spend a lot of time in outdoor environment and have the risk of becoming infected again.
Practicing certain measures can increase the chance of safety for pets and even human beings around them. These include:
- Cleaning the living area of pets at least once every week.
- Teaching children the importance of washing hands in order to prevent infection.
- Teaching children the dangers of eating soil or dirt.
- Removing all traces of animal feces from the home and surroundings. Feces should be disposed of in the trash, bagged or buried.
- Washing hands after handling pet waste.
- Not allowing children to play in regions soiled with feces of pets or other animals.
- Putting a cover on unused sandboxes to ensure that animals do not get inside and contaminate them.
- Washing hands with soap and warm water after playing with animals or pets after outdoor activities or before cooking/eating.
The presence of a strong protective layer allows Toxocara eggs the ability to survive for months or even years in appropriate living conditions. Although common disinfectants are ineffective against Toxocara eggs although high heat has been found to destroy them. Immediate removal of animal feces can help prevent infection as 2-4 weeks are necessary for eggs to get infective once they are out of the body of animals.
The eradication of T. canis infection is difficult due to the complexity of the life cycle of the microbe. However, practicing good hygiene can help reduce the risk of infection in humans.
Toxocariasis Pictures
Check out the following images associated to this disorder.
Picture 1 – Toxocariasis
Picture 2 – Toxocariasis Image
If you suspect yourself or your child to be suffering from Toxocariasis, get in touch with a medical professional to discuss the possibility of infection and undergo diagnosis, if required. As aforesaid, the condition even involves loss of vision and death in severe cases. Naturally, it is safe to seek prompt medical attention and avert the risk of all possible complications associated to the disorder and also ensure early recovery.
References:
http://www.nhs.uk/Conditions/Toxocariasis/Pages/Introduction.aspx
http://en.wikipedia.org/wiki/Toxocariasis
http://www.patient.co.uk/doctor/Toxicariasis.htm
http://emedicine.medscape.com/article/229855-overview
The post Toxocariasis appeared first on Prime Health Channel.
]]>The post Toxic Shock Syndrome appeared first on Prime Health Channel.
]]>Toxic Shock Syndrome Definition
It is an acute disorder that is characterized by shock, fever and problems with the functioning of various organs of the body.
This disorder is also referred to as Staphylococcal Toxic Shock Syndrome.
Toxic Shock Syndrome ICD9 Code
The ICD9 Code of this disorder is 040.82.
Toxic Shock Syndrome Incidence
The rate of prevalence of Streptococcal Toxic Shock Syndrome has been estimated to range between 1.2 and 7.3 in every one million patients. The incidence of Staphylococcal TSS is reportedly one in every 100,000 women who are menstruating.
Toxic Shock Syndrome Symptoms
The typical signs and symptoms of this disease include:
- Headaches
- Diarrhea
- Muscle aches
- Confusion
- Seizures
- Low blood pressure
- Nausea and vomiting
- Redness of eyes, mouth, throat
- Malaise or general or ill-feeling
- High fever, sometimes accompanied by chills
- Organ failure (usually failure of the liver and kidneys)
The condition is also characterized by the development of widespread red rash that appear as a sunburn. There is peeling of the skin of patients which occurs 1 or 2 weeks after the development of the rashes, especially on the bottom of the feet or palms of the hand.
Patients should call a doctor immediately in case of the development of any of the above mentioned symptoms of TSS. This is particularly significant if suffering women are menstruating or have just completed menstruating and have been using tampons or having a wound or skin infection. Sufferers should inform doctors about the symptoms and the duration of their persistence.
Toxic Shock Syndrome Causes
The disorder may affect any individual. Around half of all cases of TSS arise in patients who are not menstruating, including men, older women and children.
The condition results from a toxin that is produced by some forms of Staphylococcus bacteria. Toxic Shock-Like Syndrome, which is a similar syndrome, can result from Streptococcal bacteria. However, TSS may not arise due to all strep or staph infections.
The earliest cases of TSS occurred in women who used tampons during menstruation. Today, less than half of all cases of the disease are related with the usage of tampons. TSS can also occur after operations or in case of burns or skin infections.
TSS has been associated with:
- Use of superabsorbent tampons
- Wearing a contraceptive sponge or a diaphragm
- Presence of a strep or staph infection, particularly in case of healing surgical incisions or skin wounds
Medical researchers are yet in the dark regarding the exact way in which tampons are possibly responsible for the occurrence of TSS. Some doctors and researchers are of the opinion that tampons may be conducive for breeding of bacteria when superabsorbent tampons are left in position for a long duration. Others suggest that the fibers in the superabsorbent tampons can scratch the vaginal surface, making it possible for entry of bacteria or their toxins into the bloodstream.
Toxic Shock Syndrome Risk Factors
The factors that increase susceptibility to this condition include:
- Menstruation
- Having a baby recently
- Undergoing a surgery recently
- Wound infection after surgery
- Foreign bodies or packings (as used to stop nosebleeds)
- Use of tampon (especially in case of leave one inside for a long time)
- Infection by the bacterium Staphylococcus aureus (S. aureus), commonly referred to as Staph infection
Toxic Shock Syndrome Diagnosis
There is no particular diagnostic exam for the detection of this condition. This is due to the fact that no single exam can help establish the presence of TSS.
Patients may need to provide physicians with samples of their urine and blood to help them check for the presence of a strep or staph infection.
For laboratory analysis, samples from the throat, cervix or vagina may also be used.
The diagnosis depends on the following criteria:
- Low blood pressure
- Fever
- Rash, that peels after one to two weeks
- Problems with the functioning of a minimum of three organs
In certain cases, blood cultures may test positive for the growth of S. aureus.
The rapid streptococcal test can be carried out within 10 – 15 minutes. The results are positive in over 85% of sufferers with TSS resulting from Streptococcus infections. In the majority of cases, medical treatment is initiated on an emergency basis before laboratory results are available. Blood tests should be negative for rheumatologic conditions and viral infections. If the heart is involved, Electrocardiogram results may be abnormal.
Toxic Shock Syndrome Differential Diagnosis
At the time of diagnosis, physicians should ensure that patients are actually complaining of symptoms occurring due to TSS and not of any similar disorder such as:
- Cellulitis
- Drug reaction
- Gas gangrene
- Heat stroke
- Bacterial sepsis
- Bacterial pharyngitis
- Bacterial pneumonia
- Leptospirosis
- Listeria monocytogenes
- Kawasaki’s disease
- Meningococcal infections
- Hemorrhagic shock
- Infectious mononucleosis
- Rocky Mountain spotted fever
- Stevens-Johnson syndrome
- Other staphylococcal infections
- Other streptococcal infections
Doctors are likely to carry out necessary tests and medical exams to ensure the absence of the above problems in sufferers and confirm the presence of TSS.
Toxic Shock Syndrome Treatment
Patients who develop TSS are likely to be hospitalized and require antibiotic drugs. Doctors try to detect the source of infection in sufferers.
The aim of treatment is to maintain the vital functions of the body. This may involve:
- Fluid administration through a vein (IV)
- Medications to control blood pressure
- Dialysis (in case of presence of acute kidney problems)
- Intravenous gamma globulin, in acute cases
- Antibiotics for any infection (may be administered through an IV)
- Staying in the hospital intensive care unit (ICU) for monitoring
Along with antibiotics, patients are likely to receive supportive care. This would help treat the signs and symptoms of TSS. If the blood pressure of sufferers begins to drop (Hypotension), it may be stabilized with the aid of medications. Fluids may be administered to cure dehydration.
The toxins manufactured by the strep or staph bacteria and associated Hypotension may lead to kidney failure. If the kidneys fail, sufferers may need Dialysis.
Any foreign objects, like vaginal sponges, nasal packing or tampons, are removed. Sites of infection, like a surgical wound, are drained.
Toxic Shock Syndrome Rehabilitation
The rehabilitation therapy for TSS depends on any complications that occur due to the syndrome. The heart is the most susceptible organ to suffer from damage due to shock. As a result, physical therapists may develop a workout program to strengthen the heart and the lungs.
The condition also requires rehabilitation if the disorder leads to general fatigue and/or has an impact on the nervous system of patients. A gradual strengthening program may be started if a doctor determines the absence of any contraindications for physical activity.
Activities similar to aerobics aim at enhancing the ability of affected individuals to work and help build resistance to fatigue. A physical therapist is likely to address the issues of retraining and balance in case of damage to the nervous system.
When endurance is increased without symptoms like respiratory shortness, sufferers can start active light resistance training and progress to mild resistance workouts with the use of free weights and/or weight machines. Based on the general health status of sufferers, the frequency of the program tends to vary.
Toxic Shock Syndrome Prognosis
With the help of appropriate treatment, sufferers generally attain recovery within a span of two to three weeks. However, the disease can be life-threatening in a few hours. It can be fatal in up to half of all cases. Due to this reason, treatment is needed on an immediate basis in case of an occurrence of the condition.
There is risk of recurrence of this syndrome even in those patients who manage to survive.
Toxic Shock Syndrome Complications
The possible complications associated to TSS include the following problems:
- Shock
- Severe dysfunction of important organs, such as heart, liver or kidney
- Death
When bacterial toxins are released into the bloodstream, there may be abnormalities in the coagulation (clotting) of blood resulting in a loss of blood supply to various sections of the body (Disseminated Intravascular Coagulation). The dysfunction of organs occurs as a result of deficiency of blood flow. Patients may also suffer from loss of a limb due to this reason. Lung problems may result in extreme difficulty in respiration, a condition known as Adult Respiratory Distress Syndrome (ARDS). In acute cases, even death may occur.
Toxic Shock Syndrome Prevention
The occurrence of Menstrual TSS can be avoided by changing tampons on a frequent basis, at least after every 4 to 8 hours. Women should consider using the lowest absorbency tampon and try to change sanitary napkins and tampons whenever they can. They should practice complete avoidance of tampons when the flow is very light and use minipads as a substitute.
As aforesaid, there is a risk of recurrence associated with this syndrome. Those who get it can suffer from it again even after attaining recovery once. Due to this reason, those suffering from TSS or having a history of strep or staph infection should not use tampons at all.
Toxic Shock Syndrome Recovery Time
As already mentioned, patients usually take anywhere from two to three weeks for complete recovery. Heavy physical work may be prevented due to extended periods of weakness. Some amount of mental weakness may persist for a few weeks and may also reduce performance of sufferers in highly stressful situations.
Other accommodations for patients depend on how acute the damage of organ is, if any. Work restrictions tend to be minimal with complete recovery.
Toxic Shock Syndrome Pictures
The following images help you get an idea of the physical appearance of sufferers of this disorder.
Picture 1 – Toxic Shock Syndrome
Picture 2 – Toxic Shock Syndrome Image
In case you find the manifestation of symptoms of TSS such as rash and fever in yourself or anyone in your family, seek medical treatment as early as possible. As already said, the condition can be life-threatening without timely diagnosis and treatment. Due to this reason, it is important to undergo diagnosis and treatment as fast as possible.
References:
http://www.mdguidelines.com/toxic-shock-syndrome
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001676/
http://www.mayoclinic.com/health/toxic-shock-syndrome/DS00221
http://en.wikipedia.org/wiki/Toxic_shock_syndrome
The post Toxic Shock Syndrome appeared first on Prime Health Channel.
]]>The post Schistosomiasis appeared first on Prime Health Channel.
]]>Schistosomiasis Definition
It refers to an infectious condition caused by a form of parasite known as Schistosoma. The disorder is also referred to by various other names like:
- Bilharzia
- Bilharziosis
- Swimmer’s itch
- Snail fever
- Blood fluke
- Katayama fever
Schistosomiasis ICD9 Code
The ICD9 Code for this disorder is 120.
Schistosomiasis Prevalence
The disorder is not generally seen in the U.S. It is commonly reported in many subtropical and tropical regions around the world, especially of South America, Asia and Africa. Schistosomiasis is one of the most common parasitic infections in numerous regions of the world, second only to Malaria in prevalence. More than 200 million people across the world are reported to be annually affected by this disorder. It is categorized as one of the Neglected Tropical Diseases (NTDs).
Schistosomiasis History
The disorder is also known as Bilharzia, named after the doctor who described it for the first time in the mid-1800s.
Schistosomiasis Symptoms
The symptoms of this disorder tend to vary on the basis of the species of the parasite causing the condition as well as the duration of infection. In the initial stages of infection, patients tend to experience the following symptoms:
- Nausea
- Fatigue
- Abdominal pain
- Sores
- Fever
- Skin irritation
Initially, invasion of the skin may result in rashes (referred to as “Swimmer’s itch”) and itching. The Schistosome suffers destruction inside the skin in this disorder. Patients may also experience diarrhea, which may be bloody in case of some individuals. There may also be urinary problems like:
- Painful urination (Dysuria)
- Frequent urination
- Bloody urine (Hematuria)
Unless treated in time, the condition may cause patients to suffer from chronic ailments. There can be enlargement of spleen and liver. The eggs may enter the nervous system and give rise to various problems, such as seizures. The internal organs may also suffer damages.
Chronic Schistosomiasis
It refers to long-standing cases of Schistosomiasis that can arise months or even years after original exposure to the Schistosoma parasite. This happens due to the fact that adult Schistosoma worms, which are 1-2 cm in length, live in the veins surrounding the bowel and bladder for an average of duration of 3-5 years.
It can cause damage to a number of vital organs of the body, such as the kidneys, liver, bowel, bladder and genital tract.
Most people who develop chronic Schistosomiasis tend to experience its signs and symptoms several months or even years after being initially exposed to the parasite responsible for its occurrence. Chronic cases often give rise to complications in various organ systems like urinary system, liver, heart and gastrointestinal system. Those with chronic forms of the disorder may show improvement in their health condition when carefully treated with antiparasitic drugs and when their complications (associated with Schistosomiasis) are treated symptomatically.
Schistosomiasis Causes
This infectious condition may arise due to contact with water that has been contaminated by the Schistosoma parasite. Drinking from or swimming or washing in water sources contaminated by this parasite are frequently the causes of this disorder.
In its infective stages, the parasite is referred to as “Cercaria.” It freely swims in open water bodies. Upon being exposed to human skin, it burrows into the skin and matures into Schistosomula – another stage of infection. Then, it migrates to the liver and lungs where it gradually matures into adult forms.
Then, the adult worm migrates to any area of the body. This choice of body part depends on the type of parasite that it is. These regions involve:
- Bladder
- Liver
- Spleen
- Rectum
- Intestines
- Lungs
- Portal venous system (the veins responsible for transporting blood to liver from the intestines)
The symptoms of Schistosomiasis result from the natural response of the immune system to the parasitic eggs, rather than responses to the parasite itself.
Schistosomiasis Risk Factors
The risk factors of this disorder include the following:
Living in risk-prone areas
People born or living in regions, where the condition is prevalent, are naturally more susceptible to Schistosomiasis. Such individuals are naturally exposed to the Schistosoma parasite that is causative of this condition and develop the disease as a result.
Bathing or washing in the open
People washing or bathing out in the open from exposed water bodies, either due to habit or due to lack of resources, are also highly susceptible to the disease.
Being of a certain age
School-going children are at greater risk of being infected by the Schistosoma parasite as they often play or swim in water bodies that are contaminated by the microbe.
Poor hygiene
Living in or visiting areas with poor sanitation can also make an individual prone to developing this type of infection.
Schistosomiasis Diagnosis
The diagnosis of the disorder is performed by a physician or nurse. In the initial stages, this is performed by a physical examination of patients as well as a discussion about their medical history. Doctors also try to know whether or not sufferers have recently visited any tropical or subtropical region that is known for prevalence of Schistosomiasis. In regions where the infection is common, people who exhibit signs like bloody diarrhea may be assumed to be suffering from Schistosomiasis. In many cases, stools may be tested (stool examination) to check for the presence of parasitic eggs as some of these eggs are expelled by the body.
Additional diagnostic exams may include one or more of the following:
- Antibody test, to check for signs of infection
- Biopsy of tissue
- Liver function tests
- Kidney function tests
- Complete blood count (CBC) to determine any signs of anemia
- Urinalysis to look for parasite eggs
- Eosinophil count, to determine the number of some white blood cells
Schistosomiasis Differential Diagnosis
The differential diagnosis of this disorder involves isolating its symptoms from those of the following conditions that have similar signs. These include:
- Appendicitis
- Gastroenteritis
- Salmonella infection
- Urinary obstruction
- Inflammatory bowel disease
- Serum sickness
- Spinal cord infections
- Male urinary tract infection
- Female urinary tract infection
- Acute viral syndrome (including HIV)
- Pancreatitis
- Drug reactions
- Helminthic parasitic diseases
- Tropical splenomegaly
- Co-infection with malaria
- Co-infection with HIV
- Cirrhosis
- Pulmonary hypertension
- Co-infection with hepatitis B or hepatitis C
- Viral Hepatitis
- Leishmaniasis
- Gastroenteritis in Emergency Medicine
- Congestive Heart Failure and Pulmonary Edema
- Inflammatory Bowel Disease
- Myeloproliferative Disease
- Peptic Ulcer Disease
- Typhoid Fever
- Urethral Cancer
- Salmonella Infection in Emergency Medicine
Physicians should make sure that the signs exhibited by patients are not the result of any of the above-mentioned disorders.
Schistosomiasis Treatment
The treatment of this infection involves administering medicines to destroy the parasite responsible for the development of this disease. The infection is generally cured with the aid of the drug Praziquantel. However, the medicine can be difficult to obtain as well as expensive in regions where Schistosomiasis is endemic. Fortunately, many charitable organizations are working to make the drug more readily available in such areas as well as promoting adequate steps for prevention of the disorder.
In case of a severe infection or an infection that involves the brain, corticosteroids may be administered.
Cases of this disorder are usually curable with a single course of drug.
The groups that are typically targeted for the treatment of this disease include:
- Children of school-going age in endemic regions
- Risk-prone adults in endemic areas, including people engaged in occupations involving contact with contaminated water (farmers, fishermen and irrigation workers) and women engaged in domestic duties such as washing
- Whole communities living in areas considered to be highly endemic to Schistosomiasis
Schistosomiasis Prognosis
The outcome is generally good in cases where treatment is sought before acute damage or severe complications have occurred.
In the last 20 years, the disorder has been successfully controlled in a number of countries such as:
- China
- Brazil
- Egypt
- Cambodia
- Saudi Arabia
There is also evidence to suggest that the transmission of the disorder was interrupted in Morocco. In various nations, the assessment of the status of the transmission is being assessed. In the last 10 years, treatment campaigns have been upped in several Sub-Saharan nations with national coverage having been achieved in Uganda, Niger and Burkina Faso.
Schistosomiasis Complications
The possible complications of this disorder include the following:
- Seizures
- Bladder cancer
- Chronic kidney failure
- Right-sided heart failure
- Pulmonary hypertension
- Kidney and bladder obstruction
- Chronic liver damage and an enlarged spleen
- Inflammation of the colon (large intestine), along with bloody diarrhea
- Possibility of repeated blood infections, as bacteria can gain entry into the bloodstream through an irritated colon
Schistosomiasis leads to death only in rare cases. However, it can lead to illness and give rise to a variety of symptoms that are debilitating in nature.
When suffering from this disorder, affected individuals are at an elevated risk of developing bladder cancer.
Schistosomiasis Prevention
Snails are known to be an intermediate host for the Schistosoma parasite. Removing snails in water bodies used by humans can help avoid the occurrence of the infection. Other preventive measures for this disease include:
- Avoiding drinking from water bodies that are not known whether safe or not
- Avoid bathing or swimming in water bodies that are contaminated or potentially contaminated
People travelling to areas with a prevalence of Schistosomiasis should boil water before using or drinking it. They should also avoid swimming in freshwater as much as possible. Long-term steps can involve developing clean water reservoirs for use by members of communities.
Schistosomiasis Recommendations for Travelers
People travelling to endemic regions are advised to go through these preventive measures to avoid being affected by Schistosomiasis.
Things to do
Travelers should adopt the following steps to prevent the disease:
- Check whether they are going to regions with a prevalence of Schistosomiasis before traveling there.
- Ensuring that they use accommodations and water resources that are safe from potential parasite contamination. It is important to check whether a hotel, lodge or place of accommodation uses untreated water from a nearby lake as its resource.
- Swimming only in sea water or chlorinated swimming pools in areas with a prevalence of the disorder.
- Avoiding activities in endemic regions that may involve direct contact with water, such as swimming, paddling, snorkeling, diving or rafting
- Using boiled or packaged water and avoiding drinking from water sources that are open and exposed to parasitic contamination
- Visiting a general practitioner (GP) for screening tests if there is suspicion of being exposed to the Schistosoma parasite. Treatment on an early basis can stop the risk of long-term damage to the various organ systems of the body.
Things not to do
Travelers should avoid the following to prevent the occurrence of Schistosomiasis:
- Buying medications from overseas locations for curing the condition. These are often counterfeit and may produce adverse effects when taken too early or in wrong doses. The medication only works when used 8 weeks after original time of exposure to the parasite.
- Using insect repellents to avoid occurrence of infection. As yet, there is no evidence that use of repellents is effective. Also, the majority of repellents are water-soluble and likely to be washed off when in water.
- Depending on harsh towel drying of skin after contact with water. There is no reliable evidence that this is an effective way of removing the Schistosoma parasites.
- Relying on hotel staff or other travelers to know whether or not a source of water is affected. Rather, one should take steps to personally check and ensure whether or not the water resource is safe.
Schistosomiasis Pictures
Check out these images to know how sufferers of this disorder physically look like.
Picture 1 – Schistosomiasis
Picture 2 – Schistosomiasis
If you suspect yourself to be suffering from Schistosomiasis, seek medical attention as fast as possible. This would help you avoid complications of the disorder and check the condition in its very early stages, ensuring a faster recovery for yourself.
References:
http://www.nlm.nih.gov/medlineplus/ency/article/001321.htm
http://emedicine.medscape.com/article/228392-overview
http://www.wisegeekhealth.com/what-is-schistosomiasis.htm
http://en.wikipedia.org/wiki/Schistosomiasis
http://www.patient.co.uk/doctor/schistosomiasis
The post Schistosomiasis appeared first on Prime Health Channel.
]]>The post Sporotrichosis appeared first on Prime Health Channel.
]]>Sporotrichosis is a disease caused by infections of the Sporothrix schenckii fungus. This fungal disease generally affects the skin, although there are other rare forms that can affect the bones, joints, lungs and also the brain. The condition is also known as the “Rose gardener’s disease” or “Rose-thorn disease” as it can spread through roses.
Sporotrichosis Prevalence
Although the exact figures relating to the prevalence of this condition are not known, it is estimated that only 1 or 2 individuals in per million populations are affected by it, making Sporotrichosis a very rare disease.
Sporotrichosis Types
Based on the areas that are affected, various forms of this disorder exist. These include:
Skin or Cutaneous Sporotrichosis
The most common variant of this disease affects the skin or the cutaneous surface. They are most frequently found in the fingers, hands and arms.
Pulmonary Sporotrichosis
This form of the disease occurs when an individual inhales the S. schenckii spores. Patients of this disease are susceptible to pneumonia or tuberculosis.
Disseminated Sporotrichosis
When the infections of the Sporothrix schenckii fungus spread from their primary site to the secondary sites, it develops into a very rare, critical form known as disseminated Sporotrichosis. It can spread to the joint and bones (osteoarticular Sporotrichosis) or to the brain and the central nervous system (Sporotrichosis meningitis).
There are also certain other forms of the disorder, such as Endophthalmitis and Chorioretinitis.
Sporotrichosis Causes
The disorder occurs due to infections caused by the fungus called Sporothrix schenckii. It is found mostly in vegetation. Infections commonly occur when the skin gets broken while handling the plant materials like briars, rosebushes, or mulch-rich dirt.
For people involved in professions like horticulture, farming, rose gardening or maintenance of plant nurseries, Sporotrichosis can develop as a job-related disease. The fungus can enter the body through small abrasions and cuts to cause infections. Widespread or disseminated Sporotrichosis can occur in individuals having compromised immune systems as they inhale the dust that is filled with spores.
Sporotrichosis Symptoms
The infections of Sporotrichosis progresses slowly. It may take anywhere between 1 to 12 weeks for the first signs to appear after the initial contact with the fungus, although the average duration is 3 weeks. If the organism affects the skin, nodular bumps or lesions mat appear around the point of entrance as well as along the lymph nodes and blood vessels. The lesions start off as painless and small, and may range in color from being pink to purple. The lesions can become larger if left untreated and resemble boils. Small quantities of pus may come out of the lesions and nodules on an occasional basis. More lesions will start appearing, eventually developing into a chronic ulcer. Mycetomas might form under certain circumstances. These are areas where the sinus tracts are created from lymph to skin surface and they discharge granules that contain masses of organisms responsible for causing the infections. The symptoms associated with pulmonary Sporotrichosis include excessive coughing, fibrosis, cavitations and nodules of the lungs, as well as swelling of the hilar lymph nodes.
Body-wide or systemic Sporotrichosis can give rise to lung and breathing difficulties, arthritis, bone infections, as well as infections of nervous system. The tissues that surround the brain may get affected in a condition known as fungal meningitis. The disease spreads to various other parts of the body in patients who have an already compromised immune system. In such cases, the condition can prove to be life-threatening and become difficult to treat.
Sporotrichosis Diagnosis
Diagnosing Sporotrichosis can be difficult as many other conditions show signs and symptoms similar to it. A physical examination will reveal the typical sores. Commonly, a swab or a tissue sample is obtained from the infected site and is sent to lab for fungal culture. The tissue sample can be stained by using Grocott’s methenamine silver (GMS), PAS digest or Gram stain. Tissue samples are generally obtained from the skin, the sputum, the synovial fluid, or the cerebrospinal fluid. Serological tests are of little value to the diagnosis of this disorder due to its limited sensitivity and specificity.
Sporotrichosis Differential Diagnosis
A number of health conditions show signs and symptoms similar to that of Sporotrichosis. Hence, it should be differentiated from such similar disorders while determining the diagnosis of this particular condition as this will help in effective medical management. The differential diagnoses of Sporotrichosis include taking into account health disorders like:
- Yaws
- Pinta
- Syphilis
- Leprosy
- Tularemia
- Sarcoidosis
- Candidiasis
- Nocardiosis
- Tuberculosis
- Leishmaniasis
- Blastomycosis
- Histoplasmosis
- Fungal Pneumonia
- Erythema Nodosum
- Bacterial Pneumonia
- Rheumatoid Arthritis
- Paracoccidioidomycosis
- Staphylococcal Infections
- Mycobacterium Marinum
- Ulceroglandular tularaemia
Sporotrichosis Treatment
The treatment of this condition depends on the areas of the body that are affected as well as the severity of the disease. A number of treatment options are proposed for it, which include the following:
Saturated solution of potassium iodide
Although doctors are not sure how it does work, applying potassium iodide in a droplet form has been found to heal cutaneous Sporotrichosis. This generally takes anywhere between three to six months of treatment.
Antifungal drugs like Fluconazole and Itraconazole (Sporanox)
At present, the drug Itraconazole is more prevalently used to treat this disorder instead of Fluconazole. Patients having low tolerance for Itraconazole should be treated with Fluconazole.
Amphotericin B
The antifungal medication Amphotericin B is delivered intravenously. Several patients, however, find it difficult to tolerate Amphotericin B because of its potential after-effects like nausea, vomiting and fever. Lipid formulations of the Amphotericin B are generally recommended instead of the Amphotericin B deoxycholate due to its lower risks of causing any adverse effects. Severe infections occurring during pregnancy can be treated with Amphotericin B. Children having disseminated or severe diseases can be initially treated with Amphotericin B deoxycholate which can then be followed by itraconazole. Patients of Sporotrichosis meningitis can be treated with a combination of 5-fluorocytosine/Flucytosine and Amphotericin B.
Newer forms of triazoles
Posaconazole can be used as an alternate form of therapy for Sporotrichosis as its in-vitro activity is similar to the drugs itraconazole and amphotericin B. However, the correlation between clinical response and in vitro data is still insufficient to recommend drugs like Posaconazole and Voriconazole for the treatment of Sporotrichosis.
Surgery
Surgery might become necessary if there are bone infections or cavitatory nodules within the lungs.
Sporotrichosis Complications
Sporotrichosis can progress to give rise to other diseases, depending on the status of the immune system. The various health complications that may arise from this condition include:
- Arthritis
- Cellulitis
- Discomfort
- Sarcoidosis
- Pneumonia
- Tuberculosis
- Bone infections
- Lung and breathing difficulties
- Secondary skin infections like staph or strep
Affected individuals may also suffer from side effects of medications like Amphotericin B. Infections of joints and the central nervous system have been recorded but are quite rare.
Sporotrichosis Prognosis
The outcome for patients infected with this disease is normally good with treatment. It might take several months or even years to get rid of the infections and the affected areas might get scarred. Disseminated Sporotrichosis can be more difficult to manage and might require chemotherapy drugs. Individuals having a weak immune system can experience fatalistic implications if they are affected by Disseminated Sporotrichosis.
Sporotrichosis Prevention
Most cases of this disorder occur when the responsible organism enters the body through a wound or a cut in the skin while attending to vegetation containing these fungal spores. This disease can be prevented by wearing gloves and long sleeves to protect the hands while working with the soil, rose bushes, hay bales, sphagnum moss and pine seedlings.
Sporotrichosis in Animals
This fungal disease can also affect domestic as well as wild mammals such as cats, dogs and horses. Cats are normally affected by a severe form of skin Sporotrichosis, and medical personnel and other individuals should take protection while handling them to avoid catching the infection.
Sporotrichosis Pictures
These images show the condition of the skin after being affected by this disease.
Picture 1 – Sporotrichosis
Picture 2 – Sporotrichosis Image
References:
http://en.wikipedia.org/wiki/Sporotrichosis
http://www.nlm.nih.gov/medlineplus/ency/article/001338.htm
http://www.health.ny.gov/diseases/communicable/sporotrichosis/fact_sheet.htm
http://www.mycology.adelaide.edu.au/Mycoses/Subcutaneous/Sporotrichosis/
The post Sporotrichosis appeared first on Prime Health Channel.
]]>The post Rocky Mountain spotted fever appeared first on Prime Health Channel.
]]>Rocky Mountain spotted fever Definition
It is a disorder caused by a type of bacteria referred to as Ticks. The condition most frequently arises in summer and spring, particularly between early-April and early-September, when ticks are most active.
The disorder is also known by another name – Spotted fever.
Rocky Mountain spotted fever ICD9 Code
The ICD9 Code for this disorder is 082.0.
Rocky Mountain spotted fever Incidence
Around 600-1200 new cases of this disease are reported every year in the U.S. Only a minor number of individual ticks are infected. However, dense groups of infected ticks may exist in some neighborhoods or parks. The signs of the condition are more acute in men than women, although the causes are unclear. The symptoms are more severe in black individuals than in white ones.
The disorder has the highest rate of mortality in children and older individuals. Men die out of RMSF more than women.
Rocky Mountain spotted fever Symptoms
Patients of this disease tend to develop symptoms around 2-14 days after bitten by ticks. The possible signs include:
- Fever
- Chills
- Headache
- Mental confusion
- Muscular pain
- Nausea
- Vomiting
- Thirst
- Diarrhea
- Sensitivity to light
- Loss of appetite
- Hallucinations
Patients also develop rashes, which generally arise a few days after the onset of fever. The rashes first arise on the wrists and the ankles as spots of diameter ranging between 1 and 5 mm. In later stages, these spread to other regions of the body. However, around one-third of all sufferers of this disorder do not develop rashes. In other cases, the rashes might be localized or faintly noticeable. This makes it difficult for physicians to diagnose them.
Rocky Mountain spotted fever Causes
The bacterium exactly responsible for this condition is Rickettsia rickettsi, which is the cause for potentially lethal disorders in North and South America. When tick bites humans, the Rickettsia bacterium enters the body and gives rise to RMSF.
In the western U.S, the wood tick acts as the carrier for this bacterium. In the eastern side, it is carried by the dog tick. The infection is spread in South U.S and South and Central America by other ticks.
Although the disease is referred to as “Rocky Mountain spotted fever,” the majority of the recent cases of this RMSF have been reported in eastern U.S, which includes areas like:
- Maryland
- Georgia
- Virginia
- Oklahoma
- Tennessee
- North Carolina
- South Carolina
Most cases of RMSF develop in the summer and spring seasons. Of many as 2,300 cases reported in 2006, children were found to constitute the majority of sufferers.
The bacterium is unlikely to be transmitted by a tick that has been attached to an individual for a period less than 20 hours. Approximately only one in 1,000 dog ticks and wood ticks carry this bacterium.
The bacteria may also infect individuals who have a habit of removing ticks from their pets with bare hands and crushing them with fingers.
Rocky Mountain spotted fever Risk Factors
The risk factors for this condition include:
- Living in areas where the disease is prevalent
- Spending a long time in wooded or grassy regions
- Taking little or no protection from exposure to ticks
Rocky Mountain spotted fever Diagnosis
The diagnostic procedures for this condition usually include one or more of the following:
- Partial thromboplastin time (PTT)
- Complete blood count (CBC)
- Kidney function tests
- Prothrombin time (PT)
- Skin biopsy taken from the rash to check for R. rickettsii
- Urinalysis to check for blood or protein in the urine
- Antibody titer by complement fixation or immunofluorescence
However, the diagnosis is almost in all cases made on the basis of presentation of the symptoms in sufferers rather than on the results of tests.
Rocky Mountain spotted fever Differential Diagnosis
The differential diagnosis for RMSF involves ensuring that the symptoms experienced by patients are not the result of some other conditions, like:
- Infectious mononucleosis
- Kawasaki’s disease
- Bacterial endocarditis
- Disseminated gonococcal infection
- Idiopathic thrombocytopenia purpura (ITP)
- Leptospirosis
- Ehrlichiosis
- Gastroenteritis
- Lyme disease
- Rubella
- Measles
- Rickettsialpox
- Meningococcemia
- Pneumonia
- Rheumatic fever
- Scarlet fever
- Relapsing fever
- T shock syndrome
- Viral encephalitis
- Secondary syphilis
- Viral hepatitis
- Viral or bacterial meningitis
- Typhoid fever
- Typhus
- Thrombotic thrombocytopenia
Rocky Mountain spotted fever Treatment
The treatment for this disorder initially involves careful removal of tick from the surface of the skin. This is followed by use of antibiotic medications drugs to cure an infection. Those who develop RMSF are more likely to avoid complications if they are cured within 5 days after the onset of symptoms. This is precisely the reason why a doctor is likely to begin antibiotic therapy prior to receiving conclusive results for tests.
The preferred choices of treatment for this type of infection include Doxycycline or Tetracycline. However, these medications (particularly Doxycycline) are not a good choice for pregnant women. In cases of maternity, doctors may prescribe Chloramphenicol as a medicinal alternative. Pregnant women suffering from RMSF may safely consume Chloramphenicol.
There is some concern that Tetracycline and Doxycycline may stain the teeth of very young kids in whom permanent teeth have not developed. However, this discoloration is highly unusual when an affected child consumes these medications for two weeks or less. The medications are used as a first line of treatment, even for young kids.
Rocky Mountain spotted fever Prognosis
With proper treatment, doctors are usually successful in curing this type of infection. Patients may need extended sick leave. Specific accommodations or work restrictions depend on professional requirements of sufferers. Until physical stamina returns, patients may need modifying strenuous activity.
When the cure is accurate and started on an early basis, the outcome is usually good and the signs rapidly improve within 1-2 days. In the absence of proper treatment, the condition can have life-threatening consequences. Dog and cat owners are advised to seek medical attention for their pets within the first few hours of treatment. Doing this can ensure survival of pets without any long-term consequences.
Rocky Mountain spotted fever Mortality Rate
Death occurs in around 1-5% of RMSF sufferers, despite receiving medical cure. A higher rate of mortality is related with people who receive treatment after 5 days of the onset of the disorder. In untreated cases, death rate varies between 20-25%. Proper diagnosis and treatment in the initial stages are essential for preventing complications of RMSF and helping patients attain a complete recovery.
Rocky Mountain spotted fever Recovery Time
The length of recovery time associated with RMSF may be influenced by factors like:
- Age of individuals
- Delay in diagnosis or cure
- Presence of complications
- Acuteness of the disorder
Men tend to suffer from the disorder in a more acute manner, and may have a longer duration of disability.
Rocky Mountain spotted fever Complications
It is only in rare cases that RMSF patients are found to develop complications, which include:
- Nerve damage
- Loss of hearing
- Paralysis
Other possible complications include:
- Kidney failure
- Heart failure
- Lung failure
- Brain damage
- Meningitis
- Shock
- Problems in blood coagulation (clotting)
- Pneumonitis (lung inflammation)
Rocky Mountain spotted fever Prevention
The disease can be prevented by avoiding exposure to ticks. While hiking or walking in tick-infested regions, it is advisable to tuck long pants into sucks so as to offer protection to the legs. Long-sleeved shirts and shoes can also prevent tick bites. White or light clothes are preferable to wear in these regions as ticks can be more easily visible on such colors than over dark-colored garments. Easily spotted, they can be easily removed from garments.
If you spot a tick over a part of your skin, use a tweezer to pluck it carefully and throw it away. It may be useful to put an insect repellant to use. Antibiotics are not generally administered after a tick infection as less than 1% of ticks carry this form of infection.
The condition can be prevented in dogs by using tick collars.
Rocky Mountain spotted fever in Dogs
Ticks not only infect humans but also dogs. The bacterium is passed on to canines when ticks feed on the blood of dogs. The typical symptoms associated with dogs infected by the bacterium include:
- Fever
- Abnormal bleeding
- Inflammation of joints
- Respiratory difficulties
- Eye problems
- Muscle pain
- Destruction of platelets, resulting in development of bruises
Unless cured in time, the disorder can have fatal consequences. Veterinarians should be informed whether or not dogs have been in regions where tick exposure is possibly prevalent. Some dogs may be diagnosed in an incorrect manner due to the vague signs of ailment and difficulties in detecting this condition.
Although dogs cannot directly transmit the disorder to humans, they may carry ticks that may pass RMSF on to humans. Pet owners are advised to carefully check their dogs as well as cats for presence of ticks.
Is Rocky Mountain spotted fever Contagious?
This is not a contagious condition and cannot be transmitted from one individual to another. Presently, there is no vaccine that is available to prevent RMSF infection.
Rocky Mountain spotted fever Pictures
The following images can help you get an idea about the visual appearance of individuals affected by RMSF. Note the rashes on the arms and feet of sufferers presented here and how they have a distinct appearance in patients.

Picture 1 – Rocky Mountain spotted fever
Picture 2 – Rocky Mountain spotted fever Image
Contact a professional medical care provider without delay if you suspect yourself to have been bitten by a tick and exhibiting one or more signs of RMSF. The disease can often give rise to life-threatening complications. Naturally, it is essential to get in touch with a doctor at the earliest to ensure early recovery.
References:
http://www.nlm.nih.gov/medlineplus/ency/article/000654.htm
http://www.mayoclinic.com/health/rocky-mountain-spotted-fever/DS00600
http://www.mdguidelines.com/rocky-mountain-spotted-fever
http://en.wikipedia.org/wiki/Rocky_Mountain_spotted_fever
The post Rocky Mountain spotted fever appeared first on Prime Health Channel.
]]>